 Laguna Honda Admits Its Own Staff Jeopardize the Hospital Obtaining Recertification
Laguna Honda Admits Its Own Staff Jeopardize the Hospital Obtaining RecertificationJune 11, 2023
Laguna Honda Hospital Has Received Its Final Warnings
 Laguna Honda Admits Its Own Staff Jeopardize the Hospital Obtaining Recertification
Laguna Honda Admits Its Own Staff Jeopardize the Hospital Obtaining Recertification
‘By Its Own Admission, LHH Acknowledges Its Staff
Unable to Consistently Deliver Regulatory-Compliant and
Policy-Compliant Bedside Care to Its Residents
Staff Lack “Sense of Urgency” About Patient Care Plans
by Patrick Monette-Shaw
As an astute observer of Laguna Honda Hospital’s (LHH) now year-long problems seeking Federal re-certification to prevent closure of the facility noted privately, “Replacing LHH’s previous competent managers with ‘Flow-Project’-friendly, but incompetent and clueless, managers from San Francisco General Hospital and elsewhere in San Francisco’s Department of Public Health (SFDPH) led to the collapse of LHH as a venerable institution.”
 All you have to do is look at LHH’s ongoing problems receiving “Immediate Jeopardy” citations, which led to that collapse.
All you have to do is look at LHH’s ongoing problems receiving “Immediate Jeopardy” citations, which led to that collapse.
In the last issue of the Westside Observer, my colleague, Teresa Palmer, MD, reported that LHH had received notice from the Centers for Medicare and Medicaid Services (CMS) on May 18 extending the date that evictions might resume, one day before the pause of mandatory, involuntary discharges of LHH’s residents was scheduled to end on May 19. The pause has been extended to September 19, 2023 just three months from now.
But CMS noted harshly in the same letter that since LHH has already received multiple extensions to the mandatory discharges several times already, no further extension requests will be entertained, or granted. If LHH doesn’t get recertified soon, and is ordered to close completely, that’s it. Game over.
 Palmer’s May 26 article didn’t wade into the other news in CMS’ May 18 letter: That among other issues, Laguna Honda Hospital had been slapped with another “Immediate Jeopardy” (“I.J.”) regulatory violation on May 8, 2023, which had been identified three days earlier on Friday, May 5. The “I.J.” finding suggests LHH may still harbor patients it cannot provide adequate care for. It turns out the new “Immediate Jeopardy” citation (the most severe type of patient care deficiencies) involved problems with care plans for a resident who had attempted suicide in the facility not having been followed.
Palmer’s May 26 article didn’t wade into the other news in CMS’ May 18 letter: That among other issues, Laguna Honda Hospital had been slapped with another “Immediate Jeopardy” (“I.J.”) regulatory violation on May 8, 2023, which had been identified three days earlier on Friday, May 5. The “I.J.” finding suggests LHH may still harbor patients it cannot provide adequate care for. It turns out the new “Immediate Jeopardy” citation (the most severe type of patient care deficiencies) involved problems with care plans for a resident who had attempted suicide in the facility not having been followed.
It took a few days for public records to be released uncovering the timeline leading up to LHH receiving the “I.J.”
Observers wonder whether the new “I.J.” factored into CMS telling LHH in its May 18 letter that no further extensions on the pause of discharges will be considered after this most recent extension. LHH should take this as fair warning that it’s now “September 19 ... or bust.”
Uncovering the New “Immediate Jeopardy”
As it has before, LHH hid, downplayed, and minimized the new “Immediate Jeopardy” citation it received on May 8. News of the citation was effectively hidden for 10 days between May 8 and May 18, but it inadvertently came to light when unrelated news surfaced announcing CMS had finally agreed to extend the pause on patient transfers from May 19 to September 19.
 We only learned indirectly of LHH’s new “Immediate Jeopardy” citation in CMS’ May 18 letter. CMS wrote on May 18 that it had “endeavored” to notify LHH earlier — by May 8 — of CMS’ decision, but “LHH’s immediate jeopardy violation, however, delayed CMS’s decision” on the request to extend the pause on discharges. CMS asserted it had waited to “receive reasonable assurance from Laguna Honda that the facility’s immediate jeopardy had been abated.” In reality, CMS could have obtained that assurance six days earlier directly from the California Department of Public Health (CDPH), which agency had lifted the “I.J.” finding on May 12. CMS didn’t need LHH’s own “assurance” on May 14.
We only learned indirectly of LHH’s new “Immediate Jeopardy” citation in CMS’ May 18 letter. CMS wrote on May 18 that it had “endeavored” to notify LHH earlier — by May 8 — of CMS’ decision, but “LHH’s immediate jeopardy violation, however, delayed CMS’s decision” on the request to extend the pause on discharges. CMS asserted it had waited to “receive reasonable assurance from Laguna Honda that the facility’s immediate jeopardy had been abated.” In reality, CMS could have obtained that assurance six days earlier directly from the California Department of Public Health (CDPH), which agency had lifted the “I.J.” finding on May 12. CMS didn’t need LHH’s own “assurance” on May 14.
CMS was hoping to respond by May 8 to San Francisco City Attorney David Chiu’s May 3 letter requesting the extension on mandatory discharges. But CMS indicated that since LHH had apparently been notified on Friday, May 5 that the new “Immediate Jeopardy” would be delivered in writing on May 8, CMS decided to wait to respond to Chiu’s letter.
Of some interest, LHH’s acting CEO Roland Pickens had previously testified — or implied — multiple times to San Francisco’s Health Commission and the Commission’s LHH-JCC (Joint Conference Committee) meetings in April that the request to extend the pause of mandatory discharges had been submitted or conveyed to CMS. But it became clear in CMS’ May 18 letter that LHH and the City — via Chiu — had deliberately waited until May 3 before submitting a formal written request to CMS seeking the extension to the May 19 date on which discharges were scheduled to resume.
Sudden Letter Announces New Patient Care Initiative
 We also learned in CMS’ May 18 letter that Pickens submitted a letter to the U.S. Department of Health and Human Services (U.S. DHHS), which is the Federal department having control over CMS. Two days after CDPH lifted the “Immediate Jeopardy” at LHH on May 12, Pickens raced to submit a letter to DHHS and CMS on May 14 trying to reassure the Federal agencies that LHH was taking extraordinary steps to address its latest “Immediate Jeopardy” problem. Pickens did so, knowing “Immediate Jeopardy” citations can precipitate ending LHH’s “Settlement Agreement” with CMS.
We also learned in CMS’ May 18 letter that Pickens submitted a letter to the U.S. Department of Health and Human Services (U.S. DHHS), which is the Federal department having control over CMS. Two days after CDPH lifted the “Immediate Jeopardy” at LHH on May 12, Pickens raced to submit a letter to DHHS and CMS on May 14 trying to reassure the Federal agencies that LHH was taking extraordinary steps to address its latest “Immediate Jeopardy” problem. Pickens did so, knowing “Immediate Jeopardy” citations can precipitate ending LHH’s “Settlement Agreement” with CMS.
Six days after receiving the “Immediate Jeopardy” citation on May 8, Pickens’ May 14 letter suddenly announced a new $7 million-plus initiative to provide consistent and compliant care at patients’ bedsides. Importantly, it seems the new initiative was put into place because Laguna Honda had reached a damning conclusion:
“After 12+ months of significant and intensive work to ensure LHH is recertification survey ready, some LHH staff demonstrate practices that will jeopardize recertification.”
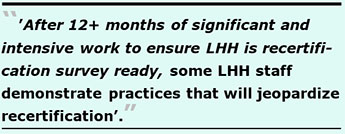 You have to wonder if the new programming is just to pass recertification, or whether the impetus is to truly improve bedside patient care! It’s fair to ask: Why was this programming not put into place 12-plus months ago, instead of only after a year of efforts to return LHH to being in substantial compliance with CMS’ regulations?
You have to wonder if the new programming is just to pass recertification, or whether the impetus is to truly improve bedside patient care! It’s fair to ask: Why was this programming not put into place 12-plus months ago, instead of only after a year of efforts to return LHH to being in substantial compliance with CMS’ regulations?
Pickens’ May 14 letter, obtained under a Westside Observer public records request, asserted that as a result of the May 8 citation, LHH decided to roll out a new patient care program called the “Consistent Care at the Bedside Initiative” (CCBI). Pickens’ letter asserted it would hire “additional consultants at a cost of over $1 million per month to observe and advise frontline staff on every floor, in every unit, for each shift.” For it’s part CMS’ May 18 letter claimed Pickens’ May 14 letter announcing the new CCBI program will “foster culture change among front-line workers [at LHH] providing bedside care.” Apparently, CMS accepted news of this new initiative at face value.
There’s a couple of notable concerns with this new initiative. First, two weeks after obtaining Pickens’ May 14 letter on May 23, the Westside Observer received a response to a subsequent records request which revealed that an additional consultant has not actually been hired at a cost of $1 million-plus per month, it’s the same consultant LHH has had since May 9, 2022 — HSAG, which has received $17 million in multiple contracts from LHH to help LHH become recertified.
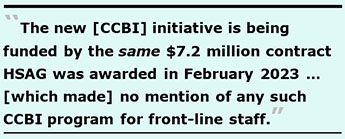 And it’s not actually a new contract. SFDPH asserts the new initiative is being funded by the same $7.2 million contract (Contract ID # 1000027889) HSAG was awarded in February 2023. One glaring problem is that when that contract was initially issued last February, there was no mention of any such CCBI program for front-line staff. Indeed, the scope of services for the contract (Appendix B-1) was titled “Laguna Honda Pre-Certification” and it listed no such “care at the bedside” initiative.
And it’s not actually a new contract. SFDPH asserts the new initiative is being funded by the same $7.2 million contract (Contract ID # 1000027889) HSAG was awarded in February 2023. One glaring problem is that when that contract was initially issued last February, there was no mention of any such CCBI program for front-line staff. Indeed, the scope of services for the contract (Appendix B-1) was titled “Laguna Honda Pre-Certification” and it listed no such “care at the bedside” initiative.
The lion’s share of the “Scope of Services” for the initial contract was for temporary consulting staffing for Nursing Home Administrator positions and Director of Nursing positions provided by HSAG at a total of $1,065,600 in billable consultant staffing hours, and consultant staffing for a Senior Quality Improvement Specialist, an Infection Preventionist, and Discharge Transfer Coaching staff at a total of $3,354,975 in billable consultant staffing — all at hourly rates of $400 per hour. There was not one mention anywhere in that contract of the CCBI program, or of any “culture change” interventions.
Apparently, the new initiative is now necessary to fix the ailing, snails-paced progress of LHH’s efforts to return to substantial regulatory compliance following its decertification 13 months ago, given stubbornly persistent problems.
It appears this sudden new initiative may be a last-ditch effort to counteract CDPH’s proposal to install its own State-hired management and crisis management team at LHH — akin to a form of receivership — to help ward off complete closure of the facility.
Downplaying Severity of the May 8 “Immediate Jeopardy”
As it has in the past, LHH and SFDPH have deliberately chosen to minimize the severity of the May 8 “Immediate Jeopardy” citation. First up was LHH acting CEO Pickens, who addressed San Francisco’s Board of Supervisors during the Board’s May 9 “Committee of the Whole” hearing on the dismal progress LHH has made toward obtaining recertification. For his part, Pickens misinformed the Supervisors (at around 1:12:56 on videotape):
“As you know, we are required by California law if there is an unusual resident or patient occurrence, we are required to report it. While they [State surveyors] came out to [investigate] one of those self-reports last week [the week of May 1 to May 5] on one of these ‘self-reports’ they found a case where a resident’s care plan was not followed appropriately that had the potential to cause harm. No harm was caused, but since they were there, they pointed that out to us. We submitted our Plan of Correction for that issue on yesterday [May 8].”
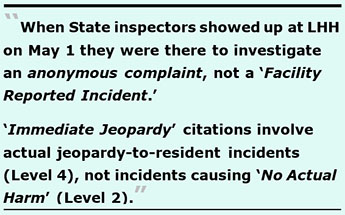 It later turned out per a “Regulatory Affairs Report” presented to the Health Commission’s LHH-JCC subcommittee on June 13 that the “self-report” Pickens had tried to pawn off wasn’t actually a self-reported “Facility Reported Incident” (“FRI”). Instead it appears that when State inspectors showed up at LHH on May 1 through May 5 they were there to investigate an anonymous complaint, not a FRI. That appears to have been what resulted in the “Immediate Jeopardy” citation. It seems someone — perhaps a family member or friend of the resident involved, or an LHH staff member — may have filed an anonymous complaint over the incident.
It later turned out per a “Regulatory Affairs Report” presented to the Health Commission’s LHH-JCC subcommittee on June 13 that the “self-report” Pickens had tried to pawn off wasn’t actually a self-reported “Facility Reported Incident” (“FRI”). Instead it appears that when State inspectors showed up at LHH on May 1 through May 5 they were there to investigate an anonymous complaint, not a FRI. That appears to have been what resulted in the “Immediate Jeopardy” citation. It seems someone — perhaps a family member or friend of the resident involved, or an LHH staff member — may have filed an anonymous complaint over the incident.
And contrary to Pickens’ attempts to downplay the incident to the Board of Supervisors, by definition “Immediate Jeopardy” citations involve actual jeopardy-to-resident incidents (Level 4 severity), not incidents causing “No Actual Harm” (Level 2 severity).
On May 16, Baljeet Sangha — a mid-level manager at the San Francisco Health Network (SFHN) who was brought in as one of two so-called “Incident Commanders” leading LHH’s recertification efforts (as if LHH’s decertification was a mere “incident”) — addressed the full San Francisco Health Commission providing a status update on LHH. He told them, in part (at 0:5:56 on videotape):
“CDPH found a case where a care plan was not being followed appropriately and that had the potential to cause harm. No harm was caused, but the potential was there so they pointed that out and our Plan of Correction was submitted last week and was accepted this past Friday [on May 12].”
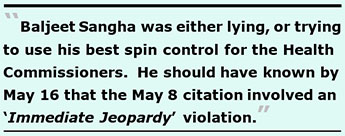 Sangha was either lying, or trying to use his best spin control for the Health Commissioners. He should have known by May 16 of Pickens’ May 14 letter to DHSS in which Pickens had acknowledged that the May 8 citation involved an “Immediate Jeopardy” violation — which is a Level 4 severity, a step above “Actual Harm” citations at Level 3 severity. The citation doesn’t appear to have involved just “potential” harm to a resident (Level 2 severity).
Sangha was either lying, or trying to use his best spin control for the Health Commissioners. He should have known by May 16 of Pickens’ May 14 letter to DHSS in which Pickens had acknowledged that the May 8 citation involved an “Immediate Jeopardy” violation — which is a Level 4 severity, a step above “Actual Harm” citations at Level 3 severity. The citation doesn’t appear to have involved just “potential” harm to a resident (Level 2 severity).
Of interest, neither Pickens nor Sangha mentioned this new $7 million-plus CCBI intervention to the Board of Supervisors on May 9, to the LHH-JCC also on May 9, or to the full Health Commission on May 16. It’s unclear whether the Health Commission even knows about this new bedside-focus intervention that LHH claimed to DHHS on May 14 it has rolled out.
Not to be outdone, Naveena Bobba — one of the Department of Public Health’s Deputy Directors — asserted in an e-mail to Supervisor Myrna Melgar on May 18 transmitting CMS’ May 18 letter extending the pause on transfers to September 19, that the incident in question had not caused harm to a patient:
“As mentioned at the LHH Hearing before the Board of Supervisor last week [on May 9] by Interim CEO Roland Pickens and at the Health Commission this past Tuesday [May 16], you’ll note the serious finding investigated by the state and that has now been closed out. There was a finding regarding a resident’s care plan not being followed appropriately that had the potential to cause harm. Importantly, no harm was caused.”
 There you have it: After struggling for over a year to get LHH staff to prepare and follow individualized care plans for its residents — a major reason LHH had been decertified for in April 2022 — the consultants have been unable to get LHH staff to implement and then follow patient’s care plans. And cavalierly, Bobba disdainfully misclassified the citation as only having the potential to cause harm (at a Level 2 severity) rather than having involved more than actual harm, which is what “Immediate Jeopardy” citations involve at severity Level 4. One wonders if Bobba understands the four severity levels.
There you have it: After struggling for over a year to get LHH staff to prepare and follow individualized care plans for its residents — a major reason LHH had been decertified for in April 2022 — the consultants have been unable to get LHH staff to implement and then follow patient’s care plans. And cavalierly, Bobba disdainfully misclassified the citation as only having the potential to cause harm (at a Level 2 severity) rather than having involved more than actual harm, which is what “Immediate Jeopardy” citations involve at severity Level 4. One wonders if Bobba understands the four severity levels.
And to delay details behind the actual event that precipitated the “Immediate Jeopardy” citations from becoming public, SFDPH and LHH have slow walked another Westside Observer public records request placed on May 23 to obtain both CDPH’s Form 2567 anonymous complaint survey inspection report and the Plan of Correction LHH claimed it had submitted by May 12 so CDPH could end the “Immediate Jeopardy” violation. Both documents may eventually shed more light on what had caused the “Immediate Jeopardy” citation.
CMS’ Other Dire Warnings
As Palmer had reported, in addition to CMS’ warning in its May 18 letter that no further extensions on the pause on transfers would be considered or awarded again, CMS also noted that although it was extending Federal Medicare and Medicaid (Medi-Cal in California) reimbursements for the remaining current residents at LHH to March 19, 2024, it also asserted that there will be no further extension of Federal reimbursements beyond that date.
Luckily, the November 10, 2022 “LHH Settlement Agreement” itself was extended from expiring at 12:01 a.m. Pacific Daylight Time on November 14, 2023 to March 19, 2024. That will give LHH more time to actually be awarded and obtain recertification status under a Medicare or Medicaid provider agreement and allow resumption of new admissions (which admissions were stopped effective in April 2022) — with the caveat that LHH may be required to resume mandatory discharges as early as September 20, 2023.
 But notably, CMS’ May 18 letter warned LHH again that any further “Immediate Jeopardy” citations may be considered a material breach under Paragraph 3-c of the “Settlement Agreement.”
But notably, CMS’ May 18 letter warned LHH again that any further “Immediate Jeopardy” citations may be considered a material breach under Paragraph 3-c of the “Settlement Agreement.”
Dire Looming Threat: State Take-Over
The May 18 letter seems to say CMS is now imposing even stricter final warnings on LHH than it did in either the November 2022 “Settlement Agreement” or in an earlier warning letter on February 1. It’s unclear whether the Health Commission and San Francisco’s Board of Supervisors get the message sent that this might be LHH’s “Last Chance Motel.”
 The letter clearly states that “California will submit a plan for resident transfers and placements by July 31, 2023, and that plan will include: a State-led crisis response team, with State-hired temporary management installed at the facility.” The May 18 letter doesn’t indicate when a State-imposed closure plan of its own might take effect, when a State-hired crisis management team might be installed at LHH, and whether either remedy might happen before September 19. That decision may come down to whether LHH receives any more “I.J.” (Level 4 severity) or “Actual Harm” (Level 3 severity) citations between now and July 31, or between now and September 19.
The letter clearly states that “California will submit a plan for resident transfers and placements by July 31, 2023, and that plan will include: a State-led crisis response team, with State-hired temporary management installed at the facility.” The May 18 letter doesn’t indicate when a State-imposed closure plan of its own might take effect, when a State-hired crisis management team might be installed at LHH, and whether either remedy might happen before September 19. That decision may come down to whether LHH receives any more “I.J.” (Level 4 severity) or “Actual Harm” (Level 3 severity) citations between now and July 31, or between now and September 19.
The CMS letter suggests this is LHH’s last chance and will now face ongoing and stricter monitoring. It sounds like LHH’s recently adopted “Revised Closure Plan” may be subsumed by a closure plan authored by the State, suggesting CMS really means business that LHH may have to close.
Left unsaid is whether the State will order LHH into some sort of a receivership, an option that appears to be a remaining remedy CMS and CDPH have left in their tool kits.
This is another slap on LHH’s management team that CDPH is apparently going install a State-hired and State-led temporary management crisis response team at LHH, presumably operating in some sort of a dual-management reporting structure.
LHH Frets Some Staff Jeopardize Recertification
In addition to Pickens’ observation in his May 14 letter to CMS that some staff continue to demonstrate practices that may jeopardize recertification, even LHH’s Quality Improvement Expert (QIE) — HSAG — has documented the same concern about LHH’s staff not being fully compliant with regulations.
One keen observer of LHH’s slow efforts at gaining recertification noted:
“Pickens’ letter to CMS confirms our worries that LHH has just not been moving fast enough … I am glad more is being done [to improve care at the bedside]. I am relieved to see the letter from Pickens. It does seems like LHH needs to move faster to not get shut down (since the problem now clearly seems to be within LHH/SFDPH). Maybe this [new programming] will help!”
She’s being optimistic. It’s not at all clear that the new CCBI program will move recertification along any faster, since LHH is planning to fund the $1 million-plus monthly initiative through at least December 2023.
The QIE’s own concerns about LHH’s staff are worrisome.
 Fourth QIE “Monitoring Report”
Fourth QIE “Monitoring Report”
Two days after Pickens admitted to DHHS on May 14 that some LHH staff may threaten LHH’s recertification, and two days before we learned in CMS’ May 18 letter that announced LHH had received yet another “Immediate Jeopardy” citation, a report surfaced on May 16 that also acknowledged LHH’s staff continue to threaten LHH’s recertification. That report — dated May 10, 2023 — was written for, and submitted to CMS, the very agency that will ultimately determine whether to accept LHH back into the Medicare and Medicaid reimbursement system. CMS is painfully aware of the problems with LHH’s staff not following Federal regulations.
On May 16, San Francisco’s Department of Public Health (SFDPH) public records staff released the Quality Improvement Expert’s (QIE) fourth monthly “Monitoring Report,” which is required by the November 2022 “LHH Settlement Agreement” between LHH, CMS, and CDPH. The “Monitoring Reports” due on the 10th day of each month are designed to report LHH’s progress towards returning to substantial compliance with federal nursing home regulations and standards of caring for patients so it can apply for CMS recertification.
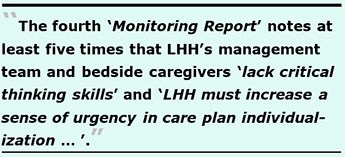 Sadly, the fourth Monitoring Report notes at least five times in four of the 11 different foundational categories of root cause problems — including Resident Quality of Care, Quality Assurance and Performance Improvement, Infection Control and Prevention, and Resident Rights and Freedom From Harm — that LHH’s management team and bedside caregivers “lack critical thinking skills” on how to correct problems at the facility.
Sadly, the fourth Monitoring Report notes at least five times in four of the 11 different foundational categories of root cause problems — including Resident Quality of Care, Quality Assurance and Performance Improvement, Infection Control and Prevention, and Resident Rights and Freedom From Harm — that LHH’s management team and bedside caregivers “lack critical thinking skills” on how to correct problems at the facility.
Also sadly, the QIE reported in its fourth report on May 10 — five months after the first RCA report dated December 1 that was submitted to CMS — “… [LHH] staff do not understand the intent of the regulations as it relates to using less restrictive alternatives prior to using restraint devices and that documentation requirements are not clearly understood by the resident care team.” The QIE also reported “LHH must increase a sense of urgency in care plan individualization … and accountability standards to improve progress [with preparing and following patients’ care plans].”
That the QIE informed CMS that there has been no sense of urgency in getting LHH’s line staff to develop and then follow patients’ care plans should alarm San Franciscans and our Board of Supervisors. That LHH staff don’t uniformly share a “sense of urgency” in returning to substantial compliance is particularly disturbing, in part because there apparently doesn’t seem to be any discipline being dispensed for non-compliant job performance.
 In the QIE’s first “Root Cause Analysis” (RCA) report dated December 1, 2022, in the major foundational Root Cause Category #2, Infection Prevention and Control, the Analysis and Findings section stated in part:
In the QIE’s first “Root Cause Analysis” (RCA) report dated December 1, 2022, in the major foundational Root Cause Category #2, Infection Prevention and Control, the Analysis and Findings section stated in part:
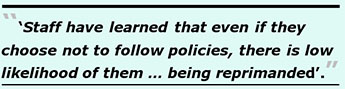
“The facility does not have a progressive disciplinary action for non-compliant behaviors. As such, staff have learned that even if they choose not to follow policies, there is a low likelihood of them losing their position or being reprimanded.”
It’s shocking some staff may have learned there are no consequences for their not complying with policies around infection prevention and control that CMS is so concerned about.
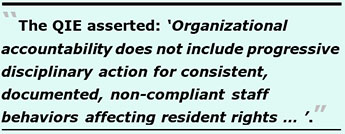 Also in the QIE’s first RCA report, in the major foundational Root Cause Category #5, Resident Rights and Freedom from Harm, Root Cause 6 involved Lack of strong accountability standards. The QIE asserted: “Organizational accountability does not include progressive disciplinary action for consistent, documented, non-compliant staff behaviors affecting resident rightsand dignity.”
Also in the QIE’s first RCA report, in the major foundational Root Cause Category #5, Resident Rights and Freedom from Harm, Root Cause 6 involved Lack of strong accountability standards. The QIE asserted: “Organizational accountability does not include progressive disciplinary action for consistent, documented, non-compliant staff behaviors affecting resident rightsand dignity.”
Wow! No accountability for staff screw-ups? No disciplinary action to weed out staff transgressors? Has that been a problem, all along? Because CMS was informed about this problem seven months ago in December, what’s taking so long to fix the problem?
Again, in the QIE’s first RCA report, in the major foundational Root Cause Category #7, Competent Staff, Training, and Quality of Care, Root Cause 3 involved Lack of accountability for mandatory educational requirements. The consultant noted “There are no consequences for employees and medical staff not completing mandatory education, resulting in some staff providing care without the tools and knowledge necessary for optimal resident outcomes.”
The QIE recommended LHH develop and implement progressive disciplinary actions for non-compliance regarding mandatory education and training.
Beyond the issue of disciplinary actions for non-compliant staff behaviors, the QIE was concerned in the major foundational Root Cause Category 6, Comprehensive Care Plans and Quality of Care in the first RCA report about the many problems with resident care plans. The QIE identified Root Cause #5, EHR [Electronic Health Record system] not optimized for SNF setting and lack of [Staff] EHR knowledge, saying “The Epic EHR utilized is not customized for the SNF setting and staff have limited knowledge of full EHR capabilities. This results in increased burden to staff to update and modify care plans, which increases the likelihood that residents have care plans with generic, acute-care–based interventions rather than comprehensive, resident-centered care plans.”
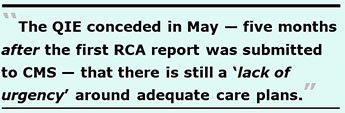 The problems with LHH’s inadequate resident care plans existed even before it was decertified in April 2022, and remained a continuing problem in May 2022 long after the consultants were brought in. Despite their best efforts, the consultants have been unable to fix the “culture” around care planning, to the point the QIE conceded in May — five months after the first RCA report was submitted to CMS — that there is still a “lack of urgency” around adequate care plans.
The problems with LHH’s inadequate resident care plans existed even before it was decertified in April 2022, and remained a continuing problem in May 2022 long after the consultants were brought in. Despite their best efforts, the consultants have been unable to fix the “culture” around care planning, to the point the QIE conceded in May — five months after the first RCA report was submitted to CMS — that there is still a “lack of urgency” around adequate care plans.
It’s too bad the QIE didn’t also recommend that LHH develop progressive disciplinary procedures for LHH staff who may believe there are no consequences for not following a resident’s care plan.
Pickens offered a ray of hope in this regards when he wrote to DHHS on May 14, in which he pointedly noted:
“LHH is committed to accountability. Accordingly, we have initiated a comprehensive investigation into all the circumstances leading to the immediate jeopardy finding. LHH will take appropriate disciplinary action against LHH personnel as warranted by the results of that investigation.”
As any parent knows, one of the hardest lessons their young children learn in life is that their own actions have consequences. It’s time LHH’s non-compliant staff relearn this basic lesson, the hard way if necessary.
LHH Waives a White Flah
 Unfortunately, Pickens’ May 14 letter addressed to officials at both DHHS and CMS who have been monitoring LHH’s progress towards obtaining recertification included another damning admission. The “SBAR” exhibit — for Situation – Background – Assessment – Recommendations — on dealing with the May 8 “Immediate Jeopardy” seems to be LHH running a white flag up the flagpole of the two agencies having the discretionary authority on whether to recertify LHH and look favorably on its application to become recertified in the coming months. The SBAR section admitted:
Unfortunately, Pickens’ May 14 letter addressed to officials at both DHHS and CMS who have been monitoring LHH’s progress towards obtaining recertification included another damning admission. The “SBAR” exhibit — for Situation – Background – Assessment – Recommendations — on dealing with the May 8 “Immediate Jeopardy” seems to be LHH running a white flag up the flagpole of the two agencies having the discretionary authority on whether to recertify LHH and look favorably on its application to become recertified in the coming months. The SBAR section admitted:
“Despite 12 months of significant investments in root cause analyses, process redesign, staff training and education, and enhanced enforcement of individual accountability, there continue to be instances where some LHH staff are at times unable to consistently and reliably deliver safe, regulatory-compliant, and policy-compliant care at the bedside, as evidenced by: our own internal key performance indicators; on-going serious regulatory survey findings (including a recent immediate jeopardy finding); and CMS QIE observations.
12 months into the journey of process improvement and regulatory compliance, it is clear by multiple measures that LHH cannot be assured of a successful CMS Recertification Survey without a focused level of targeted observation and recommended action in key areas. Specifically, we continue to see the necessary critical assessment, evaluation, communication, and thinking skills in some bedside clinicians and supervisors/managers.”
Given that the QIE has recently stated in its fourth monthly “Monitoring Report” that LHH staff have shown a lack of critical thinking skills, it’s thought there’s a typo in the last sentence above, omitting the words “a lack of” — suggesting they authors had intended to write:
“Specifically, we continue to see a lack of the necessary critical assessment, evaluation, communication, and thinking skills in some bedside clinicians and supervisors/managers.”
Pickens’ May 18 letter was sent to Stacy Sanders, a legal Counsel to Secretary Xavier Becerra at DHHS. Becerra has previously stated that since DHHS is required by law to make sure that patients are cared for safely and with the care that they’re supposed to have, DHHS has no choice by law but to say that the safety of patients must come first, and DHHS has to make sure everyone is following the rules and regulations.
 If you were the regulatory agency that will determine whether to recertify LHH, would you do so given that by LHH’s own admission as late as May 2023 — being now in its third “90-Day Monitoring Survey,” and due for it’s fifth monthly “Monitoring Report” from the QIE on June 10 — LHH is still having problems getting staff to deliver “regulatory-compliant, and policy-compliant care at the bedside” by multiple measures and indicators?
If you were the regulatory agency that will determine whether to recertify LHH, would you do so given that by LHH’s own admission as late as May 2023 — being now in its third “90-Day Monitoring Survey,” and due for it’s fifth monthly “Monitoring Report” from the QIE on June 10 — LHH is still having problems getting staff to deliver “regulatory-compliant, and policy-compliant care at the bedside” by multiple measures and indicators?
So, if you were Becerra, would you recertify a facility that as recently as May 14 acknowledged its staff is not consistently and reliably delivering safe, regulatory-compliant and policy-compliant care to patients?
Ongoing “Immediate Jeopardies”: We Will Lose LHH
After being decertified in April 2022, Laguna Honda Hospital (LHH) was forcefully warned twice — first last November, and again in February — not to get any more “Immediate Jeopardy” citations for substandard patient care violations during official State inspection on-site surveys.
 That’s because those “I.J.” citations can be material breach violations of LHH’s “Settlement Agreement,” and effectively end its attempts to become recertified. Has this misnamed “God’s Hotel” met its Last-Chance Café?
That’s because those “I.J.” citations can be material breach violations of LHH’s “Settlement Agreement,” and effectively end its attempts to become recertified. Has this misnamed “God’s Hotel” met its Last-Chance Café?
Ominously, because the first two warnings not to get any more “I.J.’s” apparently weren’t enough, in its May 18 letter CMS felt it had to warn LHH a third time:
“Thus, to ensure that funding will not be terminated under Paragraph 3 of the Agreement, Laguna Honda must ensure that no immediate jeopardy occurs at its facility for the duration of the Agreement and proposed Amendment.”
By “proposed amendment,” CMS means an extension of the “LHH Settlement Agreement” through March 19, 2024.
LHH was first warned in the November 10, 2022 LHH “Settlement and Systems Improvement Agreement” (hereinafter the “Settlement Agreement”) that among the circumstances that might constitute LHH’s material breach of the Agreement included paragraph 3-c, “CMS determines that Immediate Jeopardy to resident health and safety occurred, as that term is defined by 42 C.F.R. § 488.301.”
Then, after entering into the “Settlement Agreement,” and after the QIE’s first RCA report was submitted to CMS on December 1, that’s when LHH racked up four “Immediate Jeopardy” citations during it’s first “90-Day Monitoring Survey” that wrapped up on December 16.
Subsequently, in a February 1, 2023 letter to LHH, CMS warned the hospital for a second time that the hospital must not receive any further “I.J.” citations and must reduce the number of “Actual Harm” citations in the Level 3 severity category. CMS reminded LHH paragraph 3 of the “Settlement Agreement” provided CMS discretion to terminate the entire Agreement if LHH received any further “I.J.’s .” (LHH had received four “I.J.’s” and five “Actual Harm” citations in December.)
But along came May 8 with news LHH had again received another “I.J.”
Notably, LHH had also received four “I.J.” citations during LHH’s patient sexual abuse scandal in 2019, which set LHH on its path to being decertified in April 2022. It also racked up another 13 “I.J.’s” deficiencies during a “mock survey” inspection dress rehearsal in June 22 (after it had been decertified) before it went on to get four of the nine “I.J.” official citations six months later in December 2022.
Despite the Florence Nightingale statue having stood watch over LHH’s main entrance for 86 years as an inspiration to the hospital’s employees and its residents, LHH managed to rack up nine “Immediate Jeopardy” deficiency citations during official State survey inspections in the three years between July 12, 2019 and November 28, 2022.
Of the combined 22 “I.J.’s,” 13 of them were at the highest scope of “widespread,” rated with the letter “L” as having been pervasive in the facility. The nomenclature assesses the combined severity and scope together, abbreviated as “S/S.”
A reasonable person might have hoped the Florence Nightingale statue might have warded off further staff “I.J.” negligence. But that didn’t happen.
LHH has been mum about whether it has developed progressive disciplinary policies and procedures to deter documented non-compliant staff behaviors contributing to the facility receiving “I.J.” citations. Another separate Westside Observer public records request on this issue also remains unanswered two weeks after it was submitted.
Will LHH’s third warning not to get any further “I.J.’s” be the charm? As in, three strikes, you’re out.
After all, LHH has been holding a losing hand, and may be running out of clock.
As the San Francisco Gray Panthers advocacy group has noted: “At the rate things are going, SFDPH/LHH may not  sufficiently improve in time to avoid closure procedures and discharges for every resident beginning September 19, 2023.”
sufficiently improve in time to avoid closure procedures and discharges for every resident beginning September 19, 2023.”
And as our colleague Dr. Terry Palmer testified to San Francisco’s Health Commission on June 6, “If immediate jeopardy citations continue, we will lose Laguna Honda Hospital.”
Monette-Shaw is a columnist for San Francisco’s Westside Observer newspaper, and a retired City employee. He received a James Madison Freedom of Information Award in the “Advocacy” category from the Society of Professional Journalists–Northern California Chapter in 2012. He’s a member of the California First Amendment Coalition (FAC) and the ACLU. Contact him at monette-shaw@westsideobserver.com.