 Printer-friendly PDF file
Printer-friendly PDF fileApril 27, 2021
Confronting Out-of-County Patient Discharges
Ken Zhao's Story
 Printer-friendly PDF file
Printer-friendly PDF file
April 27, 2021
Confronting Out-of-County Patient Discharges
Ken Zhao's Story
by Patrick Monette-Shaw
Ken Zhao’s story could one day be the story of any of us. It could be me. It might be you. There, but for the grace of God, go we.
Imagine being paralyzed and on a ventilator to help you breathe.
Then imagine that a discharge planner in the long-term acute care hospital you had wound up at following discharge from Laguna Honda Hospital waltzed into your room and without any warning announced it was giving you 24-hour notice it was going to discharge you to an out-of-county facility in Sacramento or Hayward.
Imagine that your parents were told that for you to stay in San Francisco they would have to pay up to $2,400 per day, or you’d be discharged out-of-county  following the 24-hour discharge notice. That translates to $72,0000 per month, or a staggering $876,000 annually, just shy of a million bucks per year.
following the 24-hour discharge notice. That translates to $72,0000 per month, or a staggering $876,000 annually, just shy of a million bucks per year.
Forcing Ken out-of-county was preventable, had San Francisco’s Department of Public Health and the Board of Supervisors stepped up to the plate four years ago in 2017, or even earlier back in 2012.
Needing sub-acute skilled nursing care in-county close to an ICU, and close to his family and friends, is a heartbreaking challenge Ken faces, along with his health challenges.
 Luckily, following intense advocacy by well-placed advocates, Ken gained a temporary reprieve, at least for the time being, from being immediately transferred to an out-of-county sub-acute facility, because there are currently none in San Francisco. We all face the prospect of being sent out-of-county for sub-acute care.
Luckily, following intense advocacy by well-placed advocates, Ken gained a temporary reprieve, at least for the time being, from being immediately transferred to an out-of-county sub-acute facility, because there are currently none in San Francisco. We all face the prospect of being sent out-of-county for sub-acute care.
It’s sad that during San Francisco’s all-consuming COVID pandemic and subsequent lockdown that forgotten San Franciscans remain neglected in the City’s safety-net healthcare system unless they have access and connections to a coalition of healthcare advocates. Extremely ill people, and their voices,  have been all but forgotten by San Francisco government officials who appear to be blind, completely indifferent to people’s needs, or callous to their pain.
have been all but forgotten by San Francisco government officials who appear to be blind, completely indifferent to people’s needs, or callous to their pain.
Just as COVID is a respiratory condition that often requires life-sustaining ventilators — help, I can’t breathe! — so, too, are people with respiratory conditions that require ventilators or tracheostomy tubes to help safely deliver oxygen to their lungs, remove secretions from their airways, or help them breathe by bypassing an obstructed upper airway, just to keep them alive.
 The least San Francisco should do is offer those who must live on life support a chance to live in their own City.
The least San Francisco should do is offer those who must live on life support a chance to live in their own City.
CPMC’s closure of San Francisco’s only sub-acute SNF at St. Luke’s Hospital has had real consequences for people.
 Details in Ken’s story are what any one of us could face.
Details in Ken’s story are what any one of us could face.
Ken‘s Ordeal
Take a real person — Ken Zhao — to help understand how dangerous and unnecessary the lack of an in-county sub-acute Skilled Nursing Facility (SNF) is, something the Board of Supervisors have failed to correct. Sadly, Ken’s story illustrates the dire need for sub-acute SNF beds in The City.
Admission to LHH: An accident caused by a sudden-onset stroke hospitalized Ken at San Francisco General Hospital. He was in a coma and a tracheostomy tube was inserted to help him breathe, but he couldn’t speak. Ken was transferred to Laguna Honda Hospital (LHH) for skilled nursing care in 2016 when he was 34 following a pontine stroke. A pontine stroke is a cerebrovascular accident (CVA), a type of ischemic stroke that affects the pons region of the brain stem. Ischemic strokes occur when a blood clot blocks an artery leading to the brain. Pontine strokes are dangerous precisely because they frequently lead to paralysis.
Ken became quadriplegic following the brain aneurysm. Quadriplegia is paralysis from the neck down, including the trunk, legs, and arms.
Ken is an only child. His low-income parents are 70 years old, but came in to LHH almost daily to help with Ken’s exercise and suctioning of secretions in Ken’s mouth. His father, Ru Sen Zhao, is retired. Neither Mr. Zhao nor his wife speak English; they only speak Chinese. Ken was reportedly doing fine for four years while at LHH when his family could come in to assist with care giving.
The tracheostomy tube was removed after he was able to breathe again. Along came COVID, and on March 6, 2020 Mayor Breed shut down all visitation to LHH.
 His parents believe Ken was getting inadequate care from LHH’s staff, was neglected, and had deteriorated a lot inside eight months because they were locked out and couldn’t get in to care for him during LHH’s COVID lockdown between March 6, 2020 and November 15, 2020 when Ken was transferred to UCSF for acute level of care. Ken had worsened from “almost able to communicate” to being in an emergency condition.
His parents believe Ken was getting inadequate care from LHH’s staff, was neglected, and had deteriorated a lot inside eight months because they were locked out and couldn’t get in to care for him during LHH’s COVID lockdown between March 6, 2020 and November 15, 2020 when Ken was transferred to UCSF for acute level of care. Ken had worsened from “almost able to communicate” to being in an emergency condition.
This is just one example of why locking caregiving families out of nursing homes often leads to disastrous results.
 Transfer from LHH to UCSF: Ken, then 38, was transferred on November 15, 2020 from LHH to UCSF Medical Center with hypoxemic respiratory failure (not enough oxygen in his blood), urosepsis (sepsis caused by urinary tract infections), and pneumonia. The sepsis may have been caused by an infection Ken already had, and may have triggered a chain reaction throughout his body. When he improved, it became clear his ability to breathe with a tracheostomy or ventilator was marginal.
Transfer from LHH to UCSF: Ken, then 38, was transferred on November 15, 2020 from LHH to UCSF Medical Center with hypoxemic respiratory failure (not enough oxygen in his blood), urosepsis (sepsis caused by urinary tract infections), and pneumonia. The sepsis may have been caused by an infection Ken already had, and may have triggered a chain reaction throughout his body. When he improved, it became clear his ability to breathe with a tracheostomy or ventilator was marginal.
At the time Ken was transferred to UCSF, he also had a Sacral decubitus ulcer noted on admission. Decub pressure ulcers — commonly known as bed sores — are skin injuries that commonly develop on bony areas of the body caused by lying on a body part for long periods of time, resulting in skin break down. In other words, Ken had acquired the ulcerous bed sore while at LHH, which is notorious for Nursing staff not turning quads frequently while they’re in bed. It’s not known if Ken had received specialized in-bed positioning equipment following  a consult with an LHH Occupational Therapist knowledgeable about durable medical equipment to assist with positioning devices to help prevent bed sores.
a consult with an LHH Occupational Therapist knowledgeable about durable medical equipment to assist with positioning devices to help prevent bed sores.
I first learned of LHH’s on-going bed sore problems shortly after I was hired there in 1999. Prevention of decub ulcers had previously been of keen interest to the U.S. DOJ during an investigation of LHH residents’ civil rights before I was hired. It’s not known if Ken developed the bed sore after visitation by his parents was cut off soon after the COVID lockdown of LHH in March 2020. Nursing staff likely overwhelmed by COVID may not had enough time to turn patients, and may not have paid closer attention to bed sores of interest to the U.S. DOJ.
 During his stay at UCSF, Ken had poor clearance of respiratory secretions that required frequent suctioning. He had recurrent aspiration events (caused by inhaling food, an object, or fluid into his windpipe and lung) and worsening of chronic respiratory problems due to his quadriplegia. His quadriplegia caused other severe complications, including community-acquired pneumonia and sepsis caused by a urinary tract infection associated with a proteus bacteria organism from a suprapubic catheter inserted through his belly.
During his stay at UCSF, Ken had poor clearance of respiratory secretions that required frequent suctioning. He had recurrent aspiration events (caused by inhaling food, an object, or fluid into his windpipe and lung) and worsening of chronic respiratory problems due to his quadriplegia. His quadriplegia caused other severe complications, including community-acquired pneumonia and sepsis caused by a urinary tract infection associated with a proteus bacteria organism from a suprapubic catheter inserted through his belly.
While at UCSF, Ken’s main source of pain was his bed sore.
He had been admitted to UCSF with worsening dyspnea (shortness of breath), and the hypoxia (decreased oxygenation in the body tissues). Ken’s worsening and increased rates of aspiration resulted in transient hypoxia (when the brain doesn’t get adequate oxygen for a temporary period of time).
 Ken recovered from the pneumonia and pleural effusion (buildup of fluid between the tissues that line the lungs and the chest) during his stay at UCSF. But he continued having difficulty with airway clearance and required suctioning every two hours, along with pulmonary clearance. Although he recovered from his multiple infections, his overall condition was worsening because of his higher rates of aspiration causing the transient hypoxia.
Ken recovered from the pneumonia and pleural effusion (buildup of fluid between the tissues that line the lungs and the chest) during his stay at UCSF. But he continued having difficulty with airway clearance and required suctioning every two hours, along with pulmonary clearance. Although he recovered from his multiple infections, his overall condition was worsening because of his higher rates of aspiration causing the transient hypoxia.
Ken’s admission diagnosis was sepsis. His discharge diagnosis from UCSF was hypoxia. He initially didn’t want a tracheostomy or other intervention to improve his airway clearance. He wanted to be his own decision-maker, rather than his mother being his decision maker. Although he was ambivalent about asking for a Do Not Resuscitate or Do Not Intubate (DNR/DNI) order, he expressed his preference was to receive on-going care.
Discharge From UCSF to Kentfield Hospital: On January 3, 2021 following his nearly two month hospitalization at UCSF Medical Center, Ken was discharged to Kentfield Hospital, (a long-term acute care setting) on St. Mary’s San Francisco campus. A long-term acute care hospital (LTACH), Kentfield is a specialty facility designed to accommodate extended hospitalization needs of patients having complex medical issues, including patients with chronic respiratory failure. Kentfield prides itself on providing intense respiratory management.
 While at Kentfield, Ken agreed to having a tracheostomy and is now tracheostomy- and ventilator-dependent, but is alert and can communicate to a limited extent. He’s unlikely to be appropriate for care at other than a facility like Kentfield, or a sub-acute SNF, at any time in the near future.
While at Kentfield, Ken agreed to having a tracheostomy and is now tracheostomy- and ventilator-dependent, but is alert and can communicate to a limited extent. He’s unlikely to be appropriate for care at other than a facility like Kentfield, or a sub-acute SNF, at any time in the near future.
After three months at Kentfield, a discharge planner informed the Zhao family late on Thursday, April 8 that it wanted to discharge Ken, now 39, to a sub-acute facility in Sacramento or in Hayward with just 24-hour notice. If his family didn’t accept the discharge location, his parents would face Kentfield’s $2,400 daily charges. The Zhoa’s appealed the discharge notice.
Patients have the right to refuse any specific discharge placement, a right which Kentfield must honor.
Ken’s parents don’t drive or own a car, and there’s no public transportation to Sacramento, so they would be unable to visit or take care of Ken in Sacramento. Alternatively, although Hayward is accessible by BART, it would pose a long, problematic public transportation commute for Ken’s elderly parents.
 Ken and his parents — who live in District 6 represented by Supervisor Matt Haney — had wanted him returned to LHH where his parents could continue visiting, but they now apparently understand his level of care requires long-term placement in a sub-acute SNF located in a hospital having an on-site ICU, not in a long-term acute care hospital setting. Ken’s parents are afraid he will deteriorate again and potentially die if they aren’t able to visit him regularly and frequently.
Ken and his parents — who live in District 6 represented by Supervisor Matt Haney — had wanted him returned to LHH where his parents could continue visiting, but they now apparently understand his level of care requires long-term placement in a sub-acute SNF located in a hospital having an on-site ICU, not in a long-term acute care hospital setting. Ken’s parents are afraid he will deteriorate again and potentially die if they aren’t able to visit him regularly and frequently.
Since the Zhao’s speak only Chinese, Mr. Zhao’s former employer reached out to a host of healthcare advocates for assistance on behalf of Ken. The Zhao’s were referred to San Francisco’s long-term care ombudsman program and were linked up with lawyers affiliated with the California Advocates for Nursing Home Reform (CANHR), who helped the Zhao’s appeal Kentfield’s planned discharge location for Ken. Supervisor Haney’s staff helped the Zhao’s, and Supervisor Gordon Mar was also contacted for assistance, as was Congresswoman Nancy Pelosi’s office. The Zhao’s believe Mar was very kind to extend his help.
 Unfortunately, the Zhao’s first appeal of Ken’s impending discharge was denied. They were given a second 24-hour notice again late in the day on Saturday, April 10, which the Zhao family also appealed. Their second appeal was also denied on Tuesday, April 13. The Zhao’s received a third 24-hour notice late in the day on April 13.
Unfortunately, the Zhao’s first appeal of Ken’s impending discharge was denied. They were given a second 24-hour notice again late in the day on Saturday, April 10, which the Zhao family also appealed. Their second appeal was also denied on Tuesday, April 13. The Zhao’s received a third 24-hour notice late in the day on April 13.
A lawyer from CANHR, a member of Pelosi’s staff, and Adult Protective Services were in touch with Medicare and Kentfield about not discharging Ken until a sub-acute SNF could be found that his parents can visit easily, in part because of requirements to honor patient’s right to refuse any specific discharge plan until an appropriate placement is identified.
 Medicare ordered delay of Ken’s transfer for one to three days until additional placement options were identified for the Zhao family to review.
Medicare ordered delay of Ken’s transfer for one to three days until additional placement options were identified for the Zhao family to review.
Supervisor Mar’s office has been in contact with San Francisco’s Department of Public Health to see about whether SFDPH could assist in negotiating admitting Ken to Seton Medical Center’s sub-acute SNF in Daly City, which is the closest possible sub-acute SNF. Mar’s efforts to get SFDPH to contract for sub-acute beds at Seton in Daly City as a short-term solution is commendable. But such a contract would not be for in-county sub-acute SNF beds, which is the preferable and stated goal. Perhaps Mar — who was elected on November 16, 2018 and assumed office on January 1, 2019 — was unaware that Supervisor Safai had clarified on September 12, 2017 that the Board of Supervisors were looking for an in-county solutionto the complete lack of any sub-acute SNF facilities in San Francisco.
 Seton’s sub-acute SNF appears to have beds available, but it is closed to new admissions until Seton hires more staff. Even Seton would pose a longer public transportation commute for Ken’s elderly parents than public transportation to LHH.
Seton’s sub-acute SNF appears to have beds available, but it is closed to new admissions until Seton hires more staff. Even Seton would pose a longer public transportation commute for Ken’s elderly parents than public transportation to LHH.
Thankfully, Kentfield folded on April 16 and agreed to keep Ken at Kentfield until an appropriate facility is found.
Whether that will be in an in-county facility is not yet known.
 Ken and his family would not have had to face being discharged out-of-county from Kentfield, if Barbara Garcia’s efforts in 2017 and 2018 to repurpose available space at Chinese Hospital or St. Mary’s Hospital for some of San Francisco’s needed 70 sub-acute beds had been completed. If it had, Ken would have been able to move from Kentfield on St. Mary’s campus to St. Mary’s Hospital on the same campus.
Ken and his family would not have had to face being discharged out-of-county from Kentfield, if Barbara Garcia’s efforts in 2017 and 2018 to repurpose available space at Chinese Hospital or St. Mary’s Hospital for some of San Francisco’s needed 70 sub-acute beds had been completed. If it had, Ken would have been able to move from Kentfield on St. Mary’s campus to St. Mary’s Hospital on the same campus.
Ken’s ordeal is an example of how non-English speaking families who don’t know their rights get pushed around.
Brief background history may help frame Ken’s story in context.
In-County Sub-Acute Facility Vanished
 Ken’s story involves San Francisco’s almost decade-long lack of in-county sub-acute Skilled Nursing Facilities (SNF’s).
Ken’s story involves San Francisco’s almost decade-long lack of in-county sub-acute Skilled Nursing Facilities (SNF’s).
Since 2017, the Westside Observer newspaper has published at least five articles about the loss of San Francisco’s only sub-acute facility to care for people who need this level of care.
 In December 2017, the Westside Observer published my extended article, “Temporary Reprieve from Exile.” Among other details, the article noted the San Francisco Health Commission passed a resolution on September 5, 2017 indicating that the closure of CPMC’s SNF and sub-acute SNF beds would, in fact, have a detrimental effect on healthcare services in San Francisco. The Health Commission did so, adding an additional clause to its adopted resolution, stating “This Health Commission … is also concerned about the SNF and subacute capacity for future generations of San Franciscans.”
In December 2017, the Westside Observer published my extended article, “Temporary Reprieve from Exile.” Among other details, the article noted the San Francisco Health Commission passed a resolution on September 5, 2017 indicating that the closure of CPMC’s SNF and sub-acute SNF beds would, in fact, have a detrimental effect on healthcare services in San Francisco. The Health Commission did so, adding an additional clause to its adopted resolution, stating “This Health Commission … is also concerned about the SNF and subacute capacity for future generations of San Franciscans.” At the urging of Supervisors Safai and Ronen, the sub-acute SNF issue was pulled from the PSNS Committee when the full Board of Supervisors held a “Committee of the Whole” (CoW) hearing on September 12, 2017. Safai clarified the September 12 hearing was specifically to be about “in-county, in-hospital [sub-acute] solutions for San Francisco.”
At the urging of Supervisors Safai and Ronen, the sub-acute SNF issue was pulled from the PSNS Committee when the full Board of Supervisors held a “Committee of the Whole” (CoW) hearing on September 12, 2017. Safai clarified the September 12 hearing was specifically to be about “in-county, in-hospital [sub-acute] solutions for San Francisco.” The December 2017 article noted that through June 30, 2017 public records provided by SFDPH had documented that at least 1,381 San Franciscans had been discharged from San Francisco hospitals to out-of-county facilities because of a severe shortage of in-county facilities. DPH had confirmed that the out-of-county discharge data from SFGH and LHH had been generated from its SFGetCare custom database. [Note: As of March 13, 2020, the number of out-of-county discharges had climbed to 1,722, but the data was incomplete because it didn’t include additional discharges from SFGH between January 1, 2019 and March 13, 2020.]
The December 2017 article noted that through June 30, 2017 public records provided by SFDPH had documented that at least 1,381 San Franciscans had been discharged from San Francisco hospitals to out-of-county facilities because of a severe shortage of in-county facilities. DPH had confirmed that the out-of-county discharge data from SFGH and LHH had been generated from its SFGetCare custom database. [Note: As of March 13, 2020, the number of out-of-county discharges had climbed to 1,722, but the data was incomplete because it didn’t include additional discharges from SFGH between January 1, 2019 and March 13, 2020.] I also reported in December 2017 that the then-Director of Public Health, Barbara Garcia, had testified during the Board of Supervisors CoW hearing on September 12 that DPH was working with Dignity Health (not Sutter Health/CPMC) on trying to develop a sub-acute unit, but only for mental health patients. Sub-acute psychiatric care is completely different from sub-acute SNF care for people who are physically ill and need physical-medicine care. DPH did not appear to be working on solutions for sub-acute non-psychiatric patients who did not have a mental health diagnosis.
I also reported in December 2017 that the then-Director of Public Health, Barbara Garcia, had testified during the Board of Supervisors CoW hearing on September 12 that DPH was working with Dignity Health (not Sutter Health/CPMC) on trying to develop a sub-acute unit, but only for mental health patients. Sub-acute psychiatric care is completely different from sub-acute SNF care for people who are physically ill and need physical-medicine care. DPH did not appear to be working on solutions for sub-acute non-psychiatric patients who did not have a mental health diagnosis. Finally, my December 2017 article noted that it was incumbent on the Board of Supervisors to require that all hospitals in San Francisco provide data on all out-of-county discharges of San Francisco residents back to June 30, 2006 in order to gain an historical context of just how severe this problem has been.
Finally, my December 2017 article noted that it was incumbent on the Board of Supervisors to require that all hospitals in San Francisco provide data on all out-of-county discharges of San Francisco residents back to June 30, 2006 in order to gain an historical context of just how severe this problem has been. Palmer reported SFDPH estimated the City needs 70 sub-acute SNF beds but would have none when CPMC closed its sub-acute SNF at St. Luke’s, and patients who choose to receive sub-acute SNF level of care are forced to leave San Francisco. She reported SFDPH had begun discussing a partnership with all other local hospitals to re-open hospital-based regular and sub-acute SNF beds.
Palmer reported SFDPH estimated the City needs 70 sub-acute SNF beds but would have none when CPMC closed its sub-acute SNF at St. Luke’s, and patients who choose to receive sub-acute SNF level of care are forced to leave San Francisco. She reported SFDPH had begun discussing a partnership with all other local hospitals to re-open hospital-based regular and sub-acute SNF beds. In February 2019, the Observer published another of my articles (“Supervisor Yee Must Prioritize Full Spectrum”), referring to San Francisco’s severe shortage of healthcare facilities for the elderly and people with disabilities (not just Yee’s single focus on housing for senior citizens).
In February 2019, the Observer published another of my articles (“Supervisor Yee Must Prioritize Full Spectrum”), referring to San Francisco’s severe shortage of healthcare facilities for the elderly and people with disabilities (not just Yee’s single focus on housing for senior citizens). [Note: Now two-years-and-eight-months later, Dr. Colfax and DPH haven’t solved the problem we have no sub-acute beds in the City. Those three-and-a-half years can’t be blamed entirely on our one-year COVID pandemic. It’s as if there is no sense of urgency in City government. How much longer is all of this going to take? When will the City act to stop the out-of-county patient dumping, and eviction and exile?]
[Note: Now two-years-and-eight-months later, Dr. Colfax and DPH haven’t solved the problem we have no sub-acute beds in the City. Those three-and-a-half years can’t be blamed entirely on our one-year COVID pandemic. It’s as if there is no sense of urgency in City government. How much longer is all of this going to take? When will the City act to stop the out-of-county patient dumping, and eviction and exile?] In October 2019, the Westside Observer published another article by Dr. Palmer (“San Francisco and all Hospitals Need to Provide Subacute SNF Care for San Franciscans NOW”). Her article appeared five months before COVID descended on the City. Palmer reported that SFDPH restarted its effort in 2019 to identify and secure an adequate number of sub-acute SNF beds in San Francisco under public-private partnerships in existing hospital facilities, with financial support provided proportionately through contributions from private sector entities.
In October 2019, the Westside Observer published another article by Dr. Palmer (“San Francisco and all Hospitals Need to Provide Subacute SNF Care for San Franciscans NOW”). Her article appeared five months before COVID descended on the City. Palmer reported that SFDPH restarted its effort in 2019 to identify and secure an adequate number of sub-acute SNF beds in San Francisco under public-private partnerships in existing hospital facilities, with financial support provided proportionately through contributions from private sector entities. Again, before COVID came down there was talk of repurposing available space at Chinese Hospital or St. Mary’s Hospital into a sub-acute unit. But nothing ever happened. Kelly Hiramoto at SFDPH appears to be the point person on the sub-acute bed issue.
Testimony to Board of Supervisors
In addition to these five articles in the Westside Observer, public testimony was presented to the Board of Supervisors Public Safety and Neighborhood Services Committee (PSNS) in September 2019 and January 2020 before COVID came along.
 In testimony I submitted for a PSNS Committee hearing on September 26, 2019 on sub-acute facility care, I noted that on September 3, 2018 I had specifically asked then-Board President Norman Yee to introduce legislation requiring each and every private-sector and public-sector hospitals in the City to submit out-of-county discharge information by various types of long-term facilities, including a limited amount of demographic data, to DPH annually and to provide retroactive data.
In testimony I submitted for a PSNS Committee hearing on September 26, 2019 on sub-acute facility care, I noted that on September 3, 2018 I had specifically asked then-Board President Norman Yee to introduce legislation requiring each and every private-sector and public-sector hospitals in the City to submit out-of-county discharge information by various types of long-term facilities, including a limited amount of demographic data, to DPH annually and to provide retroactive data.
On September 26, 2019 both DPH and Milliman presented PowerPoint presentations to the Public Safety and Neighborhood Services Committee of the Board of Supervisors regarding sub-acute and post-acute care in San Francisco. Milliman informed the PSNS Committee during the September 26 hearing that patients who are both ventilator dependent and need dialysis have no sub-acute care options in Northern California and must go to Southern California, or outside of the state, to obtain a bed in a sub-acute care facility.
 I noted labor leader Kim Tavaglione — who I had worked with at LHH when she worked for Sal Roselli’s SEIU Local 250, and had moved on to Roselli’s United Healthcare West labor union — had reportedly been working with the Board of Supervisors, and specifically with Supervisor Ronen, to craft and introduce legislation requiring out-of-county discharge data. I noted Tavaglione — who is now the interim Executive Director of the San Francisco Labor Council — had wanted highly-detailed data about each patient discharged out-of-county, which data would have been burdensome for hospitals to produce, rather than seeking just basic data reporting.
I noted labor leader Kim Tavaglione — who I had worked with at LHH when she worked for Sal Roselli’s SEIU Local 250, and had moved on to Roselli’s United Healthcare West labor union — had reportedly been working with the Board of Supervisors, and specifically with Supervisor Ronen, to craft and introduce legislation requiring out-of-county discharge data. I noted Tavaglione — who is now the interim Executive Director of the San Francisco Labor Council — had wanted highly-detailed data about each patient discharged out-of-county, which data would have been burdensome for hospitals to produce, rather than seeking just basic data reporting.
I asked why that legislation hadn’t been submitted and enacted, and asked the PSNS Committee to direct that SFDPH identify and open 70 sub-acute SNF beds in the City rapidly. The September 26, 2019 hearing on sub-acute care was again continued to the call of the Chair of the PSNS Committee.
In testimony I submitted for a PSNS Committee hearing on January 23, 2020 on sub-acute facility care, I repeated many of the same points I had submitted to the PSNS Committee in September 2019 about the need to pass legislation requiring that San Francisco hospitals report all out-of-county discharge data. I noted that SFDPH’s Kelly Hiramoto claimed on September 26, 2019 that DPH had began a process in Fall 2018 to identify a consultant to conduct an environmental scan, and manage project selection and implementation to bring new sub-acute skilled nursing beds online. Hiramoto should have known that  former Director of Public Health Barbara Garcia had started that process a year earlier in 2017. Milliman Inc. had been chosen in June 2019 as the lead consultant for the project.
former Director of Public Health Barbara Garcia had started that process a year earlier in 2017. Milliman Inc. had been chosen in June 2019 as the lead consultant for the project.
Hiramoto made a presentation to the PSNS Committee on January 23. She reported Milliman had interviewed both hospital-based “distinct part” SNF’s and “freestanding” SNF’s (non-hospital based) to understand both current capacity and potential barriers to developing sub-acute care capacity.
Hiramoto reported that Chinese Hospital was making progress on opening 23 sub-acute care beds, and she also reported that a freestanding regular skilled nursing facility — San Francisco Health Care and Rehabilitation on Grove Street — was working toward converting regular SNF beds to sub-acute care beds. Supervisor Safai rightly noted that the City’s preference was for hospital-based sub-acute care beds to facilitate immediate transfer to an ICU if a sub-acute care patient faced emergency declines in their health to avoid transfer by ambulance to an ICU.
 Hiramoto testified on January 23 that San Francisco hospitals may have discharged between 49 to potentially 90 patients out-of-county for sub-acute care, and that in 2018 the discharge count was closer to 70.
Hiramoto testified on January 23 that San Francisco hospitals may have discharged between 49 to potentially 90 patients out-of-county for sub-acute care, and that in 2018 the discharge count was closer to 70.
To his credit, on January 23 Supervisor Safai noted that it is inhumane to ask patients to move out of the City for sub-acute care. Also to his credit, Safai asked: “Are we looking at possibly bringing those people back that we had to send out of county so that their families are closer to them and they're receiving care in the city?” It’s not clear whether SFDPH is actively working on repatriating patients dumped out-of-county for sub-acute care back to the City.
 I testified, You can’t fix what you don’t measure, and that until all public- and private-sector hospitals and other community-based healthcare providers are required to report their out-of-county discharge data to SFDPH, the City is never going to be able to fix the problem of out-of-county patient dumping due to shortages of in-county sub-acute care. What you don’t measure [by not collecting data], you can’t fix.
I testified, You can’t fix what you don’t measure, and that until all public- and private-sector hospitals and other community-based healthcare providers are required to report their out-of-county discharge data to SFDPH, the City is never going to be able to fix the problem of out-of-county patient dumping due to shortages of in-county sub-acute care. What you don’t measure [by not collecting data], you can’t fix.
The January 23, 2020 hearing on sub-acute care was yet again continued to the call of the Chair of the PSNS Committee.
Years of Inaction
CPMC’s decision to close the City’s only sub-acute Skilled Nursing Facility (SNF) in the City at St. Luke’s Hospital, has had real consequences for people.
On April 11, 2021 I placed a records request to San Francisco’s Health Commission requesting any meeting agendas since Barbara Garcia’s departure in August 2018 discussing progress on opening a replacement sub-acute SNF in any hospitals located in the City, and any documents DPH may have provided to the Health Commission since Garcia’s departure regarding DPH’s progress in identifying opening a replacement sub-acute SNF in any hospital in the City that also contained an ICU.
 The records response I received from DPH’s public records staff said that following a diligent search for public records, they had found no documents provided to the Commission regarding sub-acute services since Garcia’s departure.
The records response I received from DPH’s public records staff said that following a diligent search for public records, they had found no documents provided to the Commission regarding sub-acute services since Garcia’s departure.
On April 13, I placed a public records request to Dr. Grant Colfax, the current Director of Public Health, asking for any and all documents exchanged between SFDPH and the 11 members of San Francisco’s Board of Supervisors since August 2018 regarding DPH’s progress in identifying opening a replacement sub-acute SNF in any San Francisco hospital. I also asked for any and all documents in DPH's possession since August 2018 analyzing options to open an in-county sub-acute SNF in San Francisco, including documentation identifying the location of a replacement sub-acute SNF and the expected date on which it might eventually be opened. Colfax didn’t responded to that records request.
 There you have it; apparently Garcia’s efforts to locate and open a sub-acute SNF died on the vines following her ouster, at least as far as SFDPH and its governing Health Commission goes.
There you have it; apparently Garcia’s efforts to locate and open a sub-acute SNF died on the vines following her ouster, at least as far as SFDPH and its governing Health Commission goes.
Public records requests were also placed with Supervisors Safi and Ronen on April 11 seeking documents and e-mails between each Supervisor and DPH since August 2018 discussing progress on a possible replacement sub-acute SNF in the City, and for any Board of Supervisors meeting agendas since August 2018 on the topic of a replacement sub-acute SNF in the City.
Safai responded, but provided no records since August 2018 and failed to provide the meeting agenda for the January 23, 2020 PSNS Committee hearing on sub-acute care. In a follow-up, Safai’s legislative aides haven’t responded on whether Safai has any upcoming hearings on the issue, or any pending legislation.
Supervisor Ronen’s office responded on April 22, but provided no documents on the sub-acute SNF problem since 2018 other than the testimony I submitted to the PSNS Committee in 2019 and 2020. Her office did provide a PowerPoint presentation for a June 25, 2020 hearing on improving patient flow in SFDPH’s behavioral (mental) health system of care, given COVID. The presentation noted that COVID had not changed SFDPH’s commitment to transforming San Francisco’s behavioral health system.
 It’s too bad that COVID appears to have changed Barbara Garcia’s and SFDPH’s commitment to transforming San Francisco’s sub-acute SNF problem. Why is DPH prioritizing transforming its behavioral health system, but not transforming in-county sub-acute SNF care?
It’s too bad that COVID appears to have changed Barbara Garcia’s and SFDPH’s commitment to transforming San Francisco’s sub-acute SNF problem. Why is DPH prioritizing transforming its behavioral health system, but not transforming in-county sub-acute SNF care?
Naveena Bobba, Deputy Director of Public Health, was asked to comment for this article on what progress DPH has made since August 2018 on getting St. Mary’s Hospital or Chinese Hospital to repurpose existing unused space in their facilities for use as sub-acute SNF beds. Bobba also did not respond.
The failure to move forward on identifying a replacement sub-acute SNF cannot be blamed solely on the COVID pandemic.
 Among other questions, a relevant question is how many people who needed sub-acute SNF care have been transferred out-of-county since 2012 because they did not have a coalition of powerful healthcare advocates like Ken Zhao was lucky to have?
Among other questions, a relevant question is how many people who needed sub-acute SNF care have been transferred out-of-county since 2012 because they did not have a coalition of powerful healthcare advocates like Ken Zhao was lucky to have?
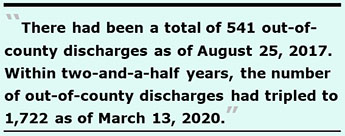
There had been a total of 541 out-of-county discharges as of August 25, 2017. Within two-and-a-half years, the number of out-of-county discharges had tripled to 1,722 as of March 13, 2020.
The Department of Public Health and the Board of Supervisors have known that the City has not had a sub-acute care facility since CPMC stopped admitting non-CPMC patients to St. Luke’s sub-acute SNF damn near a decade ago in 2012.
 Since I’ve been covering the lack of skilled nursing facilities in San Francisco for almost 20 years, please forgive me for slipping into the vernacular: DPH and the Board of Supervisors need to get off of their asses and solve the sub-acute SNF problem once and for all so the next Ken Zhao and the next family don’t have to face the possibility of being dumped out-of-county and exiled.
Since I’ve been covering the lack of skilled nursing facilities in San Francisco for almost 20 years, please forgive me for slipping into the vernacular: DPH and the Board of Supervisors need to get off of their asses and solve the sub-acute SNF problem once and for all so the next Ken Zhao and the next family don’t have to face the possibility of being dumped out-of-county and exiled.
The Zhao family provided, and consented to including, details of Ken Zhao’s medical information and his health conditions for inclusion in this article.
Monette-Shaw is a columnist for San Francisco’s Westside Observer newspaper, and a member of the California First Amendment Coalition (FAC) and the ACLU. He operates stopLHHdownsize.com. Contact him at monette-shaw@westsideobserver.com.