 November 20, 2021
November 20, 2021Another Public Health Crisis:
Why Dumping Patients Out-of-County Is Wrong
 November 20, 2021
November 20, 2021
Another Public Health Crisis:
Why Dumping Patients Out-of-County Is Wrong
by Patrick Monette-Shaw
Why is the healthcare system of a great city like San Francisco turning its back on its most vulnerable citizens who all too frequently are discharged out-of-county due to severe shortages in a wide array of healthcare facilities in the City?
As noted in September 2017, one of the world’s greatest cities should not be sending its most fragile residents into exile because they need levels of care unavailable in-county in San Francisco.
 There are great benefits to knowing how many San Francisco residents are, or have been, involuntarily discharged to out-of-county facilities, what their age ranges are, what kind of facilities they were discharged from and types of facilities they’re discharged to, and what part of San Francisco they had lived in. These are all evidenced-based measures of what types of services and types of facilities are inadequate in San Francisco.
There are great benefits to knowing how many San Francisco residents are, or have been, involuntarily discharged to out-of-county facilities, what their age ranges are, what kind of facilities they were discharged from and types of facilities they’re discharged to, and what part of San Francisco they had lived in. These are all evidenced-based measures of what types of services and types of facilities are inadequate in San Francisco.
Policymakers and elected officials need to obtain such data to guide and inform decisions about building out additional facility capacity in-county.
With modern state-of-the-art Electronic Healthcare Record (EHR) databases currently in use at all acute-care hospitals and acute psychiatric facilities in the City to track patients’ medical records, aggregate out-of-county discharge data can easily be extracted from EHR databases without breaching an individual patient’s healthcare privacy and confidentiality protected by HIPAA (Health Insurance Portability and Accountability Act). HIPAA was enacted into law in August 1996 to reform the insurance market and simplify healthcare administrative processes.
 Impacts on People Discharged Out-of-County
Impacts on People Discharged Out-of-County
There are a number of adverse impacts to people who face being dumped out-of-county, including but not limited to:
 There are no certificate-of-preference programs, or other mechanisms, to help San Franciscans dumped out-of-county return to San Francisco should additional beds in facilities appropriate to their needs be built out, or become available through vacancies via attrition.
There are no certificate-of-preference programs, or other mechanisms, to help San Franciscans dumped out-of-county return to San Francisco should additional beds in facilities appropriate to their needs be built out, or become available through vacancies via attrition.Moving physically- or mentally-challenged patients out of San Francisco is clearly detrimental to their health, given the uncertainties of a new location and skilled nursing staff. It leaves fragile patients  stranded, miles away from their families and friends.
stranded, miles away from their families and friends.
Changes to the quality of care patients receive when they are transferred to another county that has lower standards of care compared to the care they had been receiving in San Francisco, is a well known adverse effect from out-of-county transfers. This is compounded by the loss of familiar surroundings and accessibility to support from their families.
Why Out-of-County Discharges Matter
If your healthcare needs deteriorate as you age or acquire a disability and you need more care than you know how to get in your own home, or you don’t have a home, you are likely to end up a patient in an acute-care hospital. This is true for the physically ill, as well as the mentally ill. The ideal outcome of an acute hospitalization is to stabilize a patient before discharging them to a location — whether to their own home or to a specialty facility — where they can access the level of care they need.
level of care they need.
Unfortunately, acute hospital and acute psychiatric beds are both very expensive, and patients who no longer need them must leave to free the bed up for the next person. Acute-care facilities are profit-driven, even when they claim to be a non-profit hospital. They have a financial incentive to get patients in and out of an acute care hospital as quickly as possible to free up an acute-facility bed for the next patient. Hospitals work aggressively to discharge patients to a so-called “post-acute” lower level of care as a profit-driven strategy to maximize their revenues.
Where do patients go, since there are not enough services or facilities in San Francisco for them? Out of county of course, away from their families, friends, caregiver support systems, and familiar places that preserve their personhoods and quality of life.
 A report considered by both San Francisco’s Department of Public Health (SFDPH) and the San Francisco Health Commission in February 2016 — “Framing San Francisco’s Post-Acute Care Challenge” — documented that all public-sector and private-sector hospitals cited out-of-county placement as necessary to transfer patients from acute-care facilities to lower levels of care. Sadly, the report failed to even examine or recommend building out additional capacity in-county.
A report considered by both San Francisco’s Department of Public Health (SFDPH) and the San Francisco Health Commission in February 2016 — “Framing San Francisco’s Post-Acute Care Challenge” — documented that all public-sector and private-sector hospitals cited out-of-county placement as necessary to transfer patients from acute-care facilities to lower levels of care. Sadly, the report failed to even examine or recommend building out additional capacity in-county.
Unfortunately, five years ago on February 19, 2016 the San Francisco Examiner published an article discussing the “Post-Acute Care Shortage” report that was presented to the Health Commission on February 16. That article quoted then- Health Commissioner David Pating, MD — a psychiatrist and Chief of Addiction Medicine at Kaiser San Francisco Medical Center — as having said: “I hope we will consider out-of-City [i.e., out-of-county] and maybe even multi-county [discharge placement] options.”
 It was shocking to hear a psychiatrist like Pating advocate for breaking up therapeutic bonds patients had created for years with their healthcare and mental health providers by increasing out-of-county discharge placements. Pating, of all people, should have known about the emotional and therapeutic trauma patients endure when access to their caregiver support systems are abruptly severed. And it was obvious Pating didn’t understand that all along, all hospitals in San Francisco have been discharging patients to a variety of, and multiple, counties (Pating’s “multi-county” proposed solution). Thankfully, Dr. Pating is no longer a member of the Health Commission!
It was shocking to hear a psychiatrist like Pating advocate for breaking up therapeutic bonds patients had created for years with their healthcare and mental health providers by increasing out-of-county discharge placements. Pating, of all people, should have known about the emotional and therapeutic trauma patients endure when access to their caregiver support systems are abruptly severed. And it was obvious Pating didn’t understand that all along, all hospitals in San Francisco have been discharging patients to a variety of, and multiple, counties (Pating’s “multi-county” proposed solution). Thankfully, Dr. Pating is no longer a member of the Health Commission!
When it comes to patients — whether private-pay or those who rely on Medi-Cal — needing sub-acute skilled nursing facility (“sub-acute SNF”) care 24/7 for medical conditions that require ventilators, or tracheostomy care with frequent suctioning, it is best done on a hospital’s campus having an on-site ICU. All acute care hospitals other than CPMC’s own hospitals have had to transfer sub-acute patients out-of-county since 2012 when CPMC stopped admitting patients from all other hospital systems to its sub-acute SNF unit, despite it being the only such facility remaining in San Francisco.
 Then CPMC stopped accepting any new patients to its sub-acute SNF at St. Luke’s Hospital in 2017 — even from its own hospitals — leaving San Francisco without any in-county sub-acute SNF beds at all, the only county in California without such beds. Progress began in 2017 and 2018 to open new sub-acute SNF beds, but no replacement sub-acute unit has opened in the City during the past four years. For the past four years, an unknown number of new patients needing sub-acute SNF level of care have been discharged out-of-county.
Then CPMC stopped accepting any new patients to its sub-acute SNF at St. Luke’s Hospital in 2017 — even from its own hospitals — leaving San Francisco without any in-county sub-acute SNF beds at all, the only county in California without such beds. Progress began in 2017 and 2018 to open new sub-acute SNF beds, but no replacement sub-acute unit has opened in the City during the past four years. For the past four years, an unknown number of new patients needing sub-acute SNF level of care have been discharged out-of-county.
It is traumatic enough for patients who need SNF or assisted living level of care to face being placed in such types of facilities. But discharging them to another county adds to their trauma at a time when they need to feel the support of their own community and see familiar faces.
 Tip of an Iceberg?
Tip of an Iceberg?
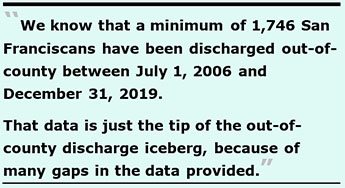
That data is just the tip of the out-of-county discharge iceberg, because of many gaps in the data provided.
Table 1: Out-of-County Discharges, July 1, 2006 — December 31, 2019
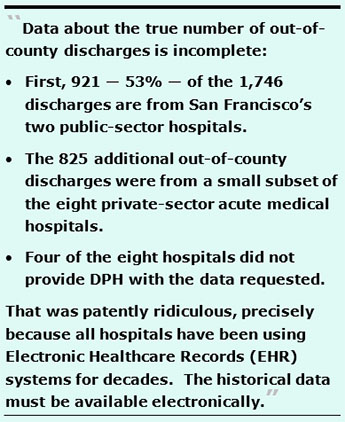
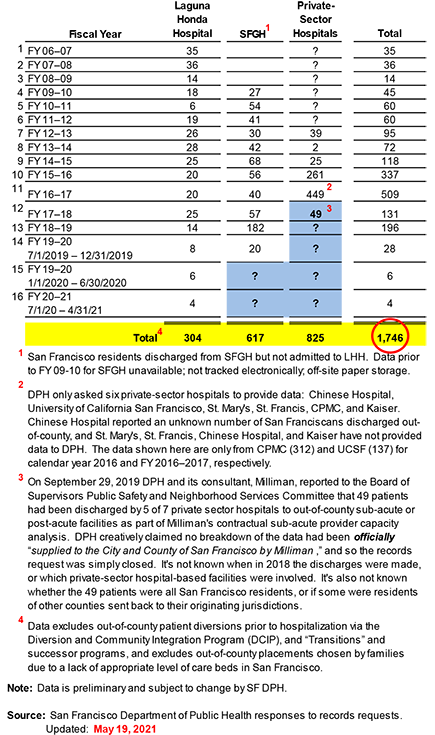
The gaps in data about the true number of out-of-county discharges is incomplete due to a variety of factors:
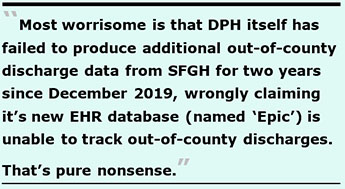 Third — and most worrisome — is that DPH itself has failed to produce additional out-of-county discharge data from SFGH for two years since December 2019, wrongly claiming that it’s new EHR database (named “Epic”) is unable to track out-of-county discharges, which as I’ve previously reported is pure nonsense (see my June 2021 article “SFDPH’s Epic Lie: A $167.4 Million Database That Couldn’t”). [Note: I will be writing a follow-up article soon because I filed and won a Sunshine complaint against DPH over SFGH’s claim Epic is unable to track out-of-county discharges.]
Third — and most worrisome — is that DPH itself has failed to produce additional out-of-county discharge data from SFGH for two years since December 2019, wrongly claiming that it’s new EHR database (named “Epic”) is unable to track out-of-county discharges, which as I’ve previously reported is pure nonsense (see my June 2021 article “SFDPH’s Epic Lie: A $167.4 Million Database That Couldn’t”). [Note: I will be writing a follow-up article soon because I filed and won a Sunshine complaint against DPH over SFGH’s claim Epic is unable to track out-of-county discharges.]Vignettes of Patients Discharged Out-of-County
A sampling of stories about patients dumped out of county include:
 therapy, occupational therapy, and speech pathology — and couldn’t be admitted to LHH. It’s well known that delays in receiving rehabilitative therapy following strokes leads to poorer patient outcomes and progressive functional decline.
therapy, occupational therapy, and speech pathology — and couldn’t be admitted to LHH. It’s well known that delays in receiving rehabilitative therapy following strokes leads to poorer patient outcomes and progressive functional decline. had told him that the longer he waited, the further he’d have to go, perhaps as far as Sacramento or Los Angeles. Ray felt he had no choice but to accept discharge to San Jose. After being transferred, Ray’s health quickly deteriorated and during one incident at the new facility, his oxygen tube disconnected. He fell out of bed and couldn’t breathe until a nurse arrived to reconnect his life-support oxygen.
had told him that the longer he waited, the further he’d have to go, perhaps as far as Sacramento or Los Angeles. Ray felt he had no choice but to accept discharge to San Jose. After being transferred, Ray’s health quickly deteriorated and during one incident at the new facility, his oxygen tube disconnected. He fell out of bed and couldn’t breathe until a nurse arrived to reconnect his life-support oxygen. He’s now surrounded in the facility by residents who are decades older and unable to communicate due to dementias. He has nobody with whom to converse. There’s no phone in his room, and whether he is brought a limited-time use phone is at the sole discretion of staff on duty. Staff have turned down his requests to use a phone multiple times. There is no on-site resident library and no resident access to computers, so Billy misses out on email, social media, music, on-line education, entertainment, and information-searching. He’d like to buy an iPad, but staff told him there’s no wi-fi, even though he can see staff down the hall working on their computers.
He’s now surrounded in the facility by residents who are decades older and unable to communicate due to dementias. He has nobody with whom to converse. There’s no phone in his room, and whether he is brought a limited-time use phone is at the sole discretion of staff on duty. Staff have turned down his requests to use a phone multiple times. There is no on-site resident library and no resident access to computers, so Billy misses out on email, social media, music, on-line education, entertainment, and information-searching. He’d like to buy an iPad, but staff told him there’s no wi-fi, even though he can see staff down the hall working on their computers.  Then there’s a patient I’ll call “Paul,” who had been living in a rent controlled unit in San Francisco. He developed problems in two of his toes, so his caregivers made an outpatient podiatry appointment at a clinic affiliated with a private-sector hospital in the City. Unfortunately, he was not prepped properly for the podiatry procedure, and not given antibiotics or a foot soaking solution after the two toenails were removed. Two days after being sent back home, Paul developed severe infections in his toes and quickly became severely disoriented, possibly from sepsis. He was admitted to a different acute care hospital in San Francisco, and spent a month-and-a-half hospitalized as doctors tried to resolve the infections in his toes, and reconstruct the top of his foot. His medical team worried the infection might migrate to other bones in his foot, and considered if they would have to amputate both toes, or possibly his whole foot.
Then there’s a patient I’ll call “Paul,” who had been living in a rent controlled unit in San Francisco. He developed problems in two of his toes, so his caregivers made an outpatient podiatry appointment at a clinic affiliated with a private-sector hospital in the City. Unfortunately, he was not prepped properly for the podiatry procedure, and not given antibiotics or a foot soaking solution after the two toenails were removed. Two days after being sent back home, Paul developed severe infections in his toes and quickly became severely disoriented, possibly from sepsis. He was admitted to a different acute care hospital in San Francisco, and spent a month-and-a-half hospitalized as doctors tried to resolve the infections in his toes, and reconstruct the top of his foot. His medical team worried the infection might migrate to other bones in his foot, and considered if they would have to amputate both toes, or possibly his whole foot. The most recent Consumer Price Index (CPI) percentage increase for all Urban Consumers in the San Francisco-Oakland-San Jose region for the 12-month period ending October 31 was 1.1%, as posted by the U.S. Bureau of Labor Statistics. That suggests Paul’s rent increase should have been a total of 6.1%, not the maximum of 10%, and certainly not the 13.4% increase the assisted living facility tried to pawn off on him. The notice of the $500 increase should have been more like a $227.53 monthly increase (to a total of $3,957.53) using the 6.1% figure, but it’s not known if these facilities can get away with creatively rounding up to the full 10% maximum, instead of the actual 6.1% CPI increase. His family is now working with healthcare advocates to obtain the lower 6.1% rate — which would be less than half of the $500 monthly rent increase.
The most recent Consumer Price Index (CPI) percentage increase for all Urban Consumers in the San Francisco-Oakland-San Jose region for the 12-month period ending October 31 was 1.1%, as posted by the U.S. Bureau of Labor Statistics. That suggests Paul’s rent increase should have been a total of 6.1%, not the maximum of 10%, and certainly not the 13.4% increase the assisted living facility tried to pawn off on him. The notice of the $500 increase should have been more like a $227.53 monthly increase (to a total of $3,957.53) using the 6.1% figure, but it’s not known if these facilities can get away with creatively rounding up to the full 10% maximum, instead of the actual 6.1% CPI increase. His family is now working with healthcare advocates to obtain the lower 6.1% rate — which would be less than half of the $500 monthly rent increase. These vignettes of patients discharged out-of-county are far from being isolated cases. Patient advocates, physicians, and mental health professionals have all reported many stories like this involving patients discharged far away, painfully.
These vignettes of patients discharged out-of-county are far from being isolated cases. Patient advocates, physicians, and mental health professionals have all reported many stories like this involving patients discharged far away, painfully.
Canaries in the Coal Mine
 I began my quest for out-of-county discharge data after badgering the Laguna Honda Hospital Joint Conference Committee (LHH-JCC) — a subcommittee of the San Francisco Health Commission made up of Health Commissioners and senior staff of LHH — for months during 2012 and 2013 to publicly release aggregate data on the number of LHH patients discharged out of county.
I began my quest for out-of-county discharge data after badgering the Laguna Honda Hospital Joint Conference Committee (LHH-JCC) — a subcommittee of the San Francisco Health Commission made up of Health Commissioners and senior staff of LHH — for months during 2012 and 2013 to publicly release aggregate data on the number of LHH patients discharged out of county.
The first trickle of data I obtained was for 28 LHH patients discharged out of county during FY 2013–2014. SFDPH eventually produced retrospective out-of-county discharge data going back to July 1, 2006 and had been providing periodic updates about out-of-county discharge data up until the end of 2019, just before COVID came along in March 2020. That’s when SFDPH and SFGH creatively began claiming it’s $167.4 million Epic replacement EHR database is unable to track out-of-county discharges.
The takeaway here is that the known 1,746 out-of-county discharges to date represent canaries in the coal mine. We’re seeing just the tip of a very, very large out-of-county discharge iceberg submerged below the surface of the water that is now leaking into the coal mine. The actual number is certainly likely far, far higher. Without adequate reporting and repercussions, patient dumping of San Franciscans out-of-county following hospitalization is certain to keep increasing.
We must not lose sight of just how severe the out-of-county discharge epidemic has grown — which is now a public health crisis. If San Francisco does not add additional in-county capacity quickly, as our aging population increases there will be many, many more people simply evicted, exiled, and dumped out of county.
 Members of San Francisco’s Board of Supervisors have been asked by a coalition of patient advocates for over four years to introduce and pass an Ordinance requiring that all hospitals in the City report aggregate data annually to SFDPH about San Franciscans discharged out-of-county. The Public Safety and Neighborhood Services Committee of our Board of Supervisors will soon hold a hearing on a very limited and currently inadequate draft Ordinance. As of this writing, the draft legislation requires hospitals to report out-of-county discharges only for those needing sub-acute SNF care placement.
Members of San Francisco’s Board of Supervisors have been asked by a coalition of patient advocates for over four years to introduce and pass an Ordinance requiring that all hospitals in the City report aggregate data annually to SFDPH about San Franciscans discharged out-of-county. The Public Safety and Neighborhood Services Committee of our Board of Supervisors will soon hold a hearing on a very limited and currently inadequate draft Ordinance. As of this writing, the draft legislation requires hospitals to report out-of-county discharges only for those needing sub-acute SNF care placement.
The legislation must be amended to require reporting of all categories of out-of-county discharges stratified by all types of facilities San Franciscans are discharged to, not just to sub-acute SNFs’s, among other sorely-needed amendments.
Watch this space.
Monette-Shaw is a columnist for San Francisco’s Westside Observer newspaper, and a member of the California First Amendment Coalition (FAC) and the ACLU. He operates stopLHHdownsize.com. Contact him at monette-shaw@westsideobserver.com.