 July 5, 2022
July 5, 2022Laguna Honda Hospital — The Rest of the Story
LHH Cuts 120 Beds, Hires Management Fat
 July 5, 2022
July 5, 2022
Laguna Honda Hospital — The Rest of the Story
LHH Cuts 120 Beds, Hires Management Fat
Will Laguna Honda Solve Its Problems by
Eliminating 120 Additional Patient Beds and
Dumping Even More Patients Out-of-County?
by Patrick Monette-Shaw
The potential threat of closing Laguna Honda Hospital (LHH), as Westside Observer readers are likely aware of, is a result of losing eligibility for the Centers for Medicare and Medicaid (CMS) reimbursement program for low-income elderly and disabled San Franciscans. This would be a disaster for patients, families, and their beloved skilled nursing facility, given the excellent recent reporting on June 22 by Dr. Derek Kerr.
This article supplements Dr. Derek Kerr’s current article in the July 5 edition of the Westside Observer.
CMS halted new admissions to LHH on April 14, is only continuing to reimburse the City for LHH’s patients though September 15, and has tied LHH’s efforts to become CMS recertified to LHH’s ability to demonstrate its progress toward discharging all 686 patients LHH had as of May 6 — 96.5% of whom are on Medi-Cal — before September 15.
LHH’s census of 686 patients as of May 6 were noted in LHH’s Notification of Closure and Patient Transfer and Relocation Plan dated May 13, 2022. Actually, LHH’s census as of October 14, 2021 was noted to have been 710, but as of June 26, 2022 the census dropped to 644, suggesting the census has dropped by 66 in the past six months. That’s significant lost revenue for LHH.
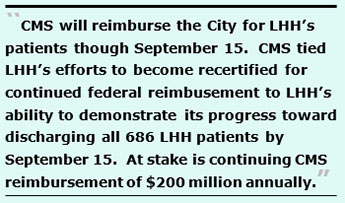 It’s all but guaranteed LHH will not be able to find skilled nursing facilities that accept Medi-Cal patients either within the City, in the nine neighboring Bay Area counties, or even in-state by September 15, since few nursing homes do.
It’s all but guaranteed LHH will not be able to find skilled nursing facilities that accept Medi-Cal patients either within the City, in the nine neighboring Bay Area counties, or even in-state by September 15, since few nursing homes do.
Even though that crisis is just beginning and nowhere near complete, another problem has emerged overnight on June 30: LHH has suddenly decided to eliminate 120 of its current 769 patient beds.
Imminent Closure of 120 of LHH’s Beds
A source informed the Westside Observer at 10:42 p.m. on Thursday, June 30 that LHH’s Interim CEO, Roland Pickens, wrote to LHH staff on June 30 announcing an immediate reorganization of LHH on July 1, 2022, claiming that CMS is “requiring” a bed reduction of 120 beds, which is a 15.6 percent change decline from 769 beds to just 649.
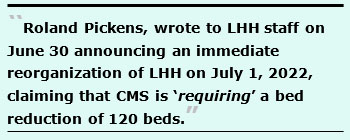 The reason for the elimination of 120 beds— that Pickens claimed was required by CMS — is addressed in detail, below, and needs immediate attention by the Board of Supervisors
The reason for the elimination of 120 beds— that Pickens claimed was required by CMS — is addressed in detail, below, and needs immediate attention by the Board of Supervisors
That reduction comes on top of the downsizing of LHH from 1,200 beds to just 780 beds in the replacement hospital that opened in 2010. The elimination of those 420 patient beds in the new Patient Towers represented a 35 percent change decline in LHH’s bed capacity in 2010. Combined, the reduction from 1,200 long-term care beds at LHH to just 649 as of July 1 amounts to a 46 percent change decline.
 There have been reports this week touting that LHH represents 34% of all skilled nursing facility (SNF) beds in San Francisco. That may have been based on a 2016 report titled “Framing San Francisco’s Post-Acute Care Challenge,” which reported there were 2,542 skilled nursing beds in San Francisco (presumably after the 420 beds were eliminated from the LHH rebuild project). However, for LHH to represent 34% of all SNF beds in the City, the denominator (the total number of beds) appears to have declined by 282 SNF beds in the past six years since the 2016 reports was published. That suggests LHH’s remaining 649 SNF beds will represent just 28.7% of all SNF beds in the City, not 35%.
There have been reports this week touting that LHH represents 34% of all skilled nursing facility (SNF) beds in San Francisco. That may have been based on a 2016 report titled “Framing San Francisco’s Post-Acute Care Challenge,” which reported there were 2,542 skilled nursing beds in San Francisco (presumably after the 420 beds were eliminated from the LHH rebuild project). However, for LHH to represent 34% of all SNF beds in the City, the denominator (the total number of beds) appears to have declined by 282 SNF beds in the past six years since the 2016 reports was published. That suggests LHH’s remaining 649 SNF beds will represent just 28.7% of all SNF beds in the City, not 35%.
That also suggests that if 282 beds had been lost citywide in the past six years and LHH is now poised to eliminate an additional 120 SNF beds, that portends 402 SNF beds will have been lost since 2016 — almost as many as the 420 SNF beds removed from the LHH rebuild in 2010.
No wonder so many SNF patients have already been discharged out-of-county. We do know that between July 1, 2006 and December 31, 2019 there have been a minimum of 1,746 out-of-county discharges, albeit that represents just a fraction of the discharges given large gaps in unreported data. But because SFDPH now claims its new Electronic Health Record (EHR) system named Epic can’t identify how many out-of-county discharges there have been between SFGH and LHH since 2019, and because SFDPH hasn’t provided updated discharge data from the City’s private sector hospitals since July 1, 2018, we have no idea how many more than 1,746 out-of-county discharges there have been during the past 16 years.
Sadly, we do know that with CMS’ requirement that LHH needs to discharge all 686 residents it had as of May 6 or risk not being recertified for CMS reimbursement, the number of out-of-county discharges will continue to climb sharply.
 Change Pickens Announced on June 30: Hiring Nursing Home Administrators
Change Pickens Announced on June 30: Hiring Nursing Home Administrators
Pickens' letter announced other substantial changes being implemented immediately, including hiring a Licensed Nursing Home Administrator (NHA) and an Assistant Nursing Home Administrator (ANHA). Pickens claimed:
“The NHA and ANHA will be advising and supporting members of the Laguna Honda senior management team (CEO, Administrative Director 1 and Administrative Director 2) and teaching these members of the senior management team how to incorporate and implement the roles of NHA and ANHA into the day-to-day operations of our skilled nursing facility, with a focus on CMS regulatory compliance and patient safety.”
 It's unclear who the two “Administrative Directors” Pickens was referring to are.
It's unclear who the two “Administrative Directors” Pickens was referring to are.
What Pickens didn’t note in the body of his June 30 letter, is that an organizational chart he included shows that the NHA position will report to LHH’s CEO (currently Pickens in an Interim CEO capacity), that is marked on the org chart as “No Supervision.” Presumably the NHA position will be advisory, and not supervise any subordinate direct reports.
One would expect that LHH’s Director of (DON) Nursing and two Assistant Director’s of Nursing would report to the new Nursing Home Administrator position. How can Pickens or Grant Colfax hope to improve LHH’s organizational structure, if the NHA position will not supervise direct reports?
This is patently ridiculous. My Aunt “Punky” (my father’s sister) was a NHA administrator, and she didn’t report to a CEO of a nursing home. She served essentially as the facility’s CEO.
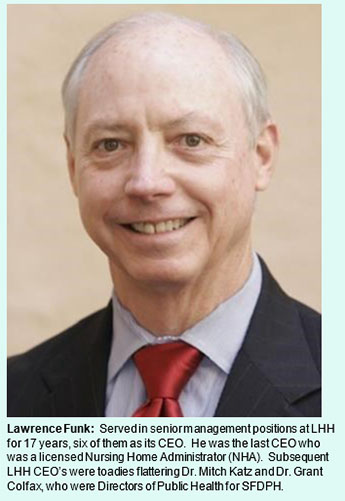
 What’s more, LHH’s last licensed NHA — Lawrence Funk — was actually LHH’s CEO. In essence, he supervised the entire hospital, albeit through layers of direct reports.
What’s more, LHH’s last licensed NHA — Lawrence Funk — was actually LHH’s CEO. In essence, he supervised the entire hospital, albeit through layers of direct reports.
An Historical Perspective
Funk had joined LHH in 1987, and served in senior management positions at LHH for 17 years, including six years as LHH CEO between 1998 and 2004. But when then-Director of Public Health Mitch Katz introduced his disastrous “flow project” in 2004 shunting angry, able-bodied and violent behavioral health male patients from SFGH and forced LHH to accept them without screening by LHH’s physician Screening Committee, Funk — himself an experienced NHA — bravely stood up to Katz and objected, but was soon replaced because of his objections to violent behavioral health patients not screened prior to admission by LHH admitting physicians. He was the last CEO at LHH to actually hold a NHA license. It should be noted that while Funk served as CEO, LHH passed all of its CMS surveys without ever losing CMS certification and reimbursement.
Katz appointed John Kanaley as Funk’s replacement in November 2004. Kanaley’s prior job experience was in “facilities management,” not hospital administration. He had served for 14 years in facilities management in SFGH’s Plant Services Department. Kanaley had earned a master’s degree in public health in 2001 — just three years before being appointed LHH’s executive administrator — by authoring his thesis involving evaluation of hazardous waste operations and removal. Many people believed Kanaley was sent to perform hazardous employee removal of LHH’s staff. Kanaley had no experience whatsoever running a skilled nursing facility, and certainly no experience or training in running a 1,200-bed nursing home having approximately 1,500 employees.
 As an LHH history reminder, in March 2004 Katz launched his misguided attempt to convert LHH into a “psychosocial rehabilitation center for the urban poor” by instituting his notorious “flow project” to divert patients being discharged from SFGH into LHH. Katz had unilaterally changed LHH’s admissions policy over the strong objections of LHH doctors concerned about patient safety. Katz’s botched plan was eventually halted by then-Mayor Gavin Newsom and then-District 7 Supervisor Sean Elsbernd.
As an LHH history reminder, in March 2004 Katz launched his misguided attempt to convert LHH into a “psychosocial rehabilitation center for the urban poor” by instituting his notorious “flow project” to divert patients being discharged from SFGH into LHH. Katz had unilaterally changed LHH’s admissions policy over the strong objections of LHH doctors concerned about patient safety. Katz’s botched plan was eventually halted by then-Mayor Gavin Newsom and then-District 7 Supervisor Sean Elsbernd.
When news surfaced Katz had forced Funk out, 415 LHH staff — including nurses, certified nursing assistants, social workers, activity therapists, dieticians, physical therapists and occupational therapists, hospital volunteers, psychologists, and clerical and secretarial employees, among others — signed a petition to the then-president of the Health Commission, Edward Chow, MD urging that Funk be restored immediately to his position as CEO. Chow himself advocated with Katz to return Funk to his position as LHH CEO.
Another 32 members of LHH’s Medical Services Department of doctors and psychiatrists signed a separate petition to Dr. Katz and the full San Francisco Health Commission, including Dr. Chow, expressing their wholehearted support of Funk, and urging Katz re-instate Funk as CEO. Within weeks of Kanaley’s appointment, a contingent of LHH’s high-level senior administrators met with Dr. Katz regarding concerns about Kanaley’s appointment and lack of credentials, experience, and qualifications. Katz reportedly told the contingent it didn’t matter because he wanted somebody who would “kick the [LHH] doctor’s asses.”
Kanaley wasn’t the first, and not last, LHH CEO to not hold a NHA license. When Kanaley dropped dead suddenly in 2009, Katz appointed Mivic Hirose, RN as LHH’s CEO. Hirose wasn’t licensed as an NHA, either, but she obediently tried to support Katz’s plan to turn LHH into a psychosocial rehabilitation facility to protect Katz’s flow project.
 In 2005, a ruckus ensued over implementing a “psycho-social rehabilitation” model of care that had been exported to LHH by Mozietta Henley, RN, PhD who was shunted from the former Mental Health Rehabilitation Facility (MHRF) on the grounds of SFGH to LHH, toting along with her, her “BioPsychoSocialSpirtual” (BPSS) model of care proposal that was never tested — and never implemented — at the MHRF. (And never really implemented at LHH either.)
In 2005, a ruckus ensued over implementing a “psycho-social rehabilitation” model of care that had been exported to LHH by Mozietta Henley, RN, PhD who was shunted from the former Mental Health Rehabilitation Facility (MHRF) on the grounds of SFGH to LHH, toting along with her, her “BioPsychoSocialSpirtual” (BPSS) model of care proposal that was never tested — and never implemented — at the MHRF. (And never really implemented at LHH either.)
Henley’s model of care comically became the impetus for a small California Health Care Foundation $50,000 grant Hirose was awarded for “Social Rehabilitation” along with my then-boss, Dr. Lisa Pascual, Chief of physical medicine Rehabilitation Services for LHH — to curry favor with Katz.
[I was there and witnessed it all: Hirose’s January 2005 grant — which created a ruckus at City Hall — ended up a notorious flop, probably an embarrassment to the California Health Care Foundation. I deliberately didn’t try to polish or proofread the Nursing Team’s final grant PowerPoint presentation as one of the five clinical teams on the grant, or help make it look like scientific research, as I did for the other four sub-teams. I chose not to, because their final presentation had focused mostly using photos of the Nursing Team enjoying their grant-funded catered lunches, and was merely word salad.]
It should also be noted that during Kanaley’s and Hirose’s tenures as CEO, LHH also eventually passed all of their CMS surveys and re-survey’s without ever losing CMS certification and reimbursement.
 Readers may recall Hirose was forced out in June 2019 after serving as LHH CEO for a decade when the LHH patient sexual abuse scandal erupted. She was replaced by Michael Phillips, FACHE — a board-certified Fellow of the American College of Healthcare Executives. Phillips also didn’t hold a NHA license, and like Kanaley, Phillips had no experience running a skilled nursing facility.
Readers may recall Hirose was forced out in June 2019 after serving as LHH CEO for a decade when the LHH patient sexual abuse scandal erupted. She was replaced by Michael Phillips, FACHE — a board-certified Fellow of the American College of Healthcare Executives. Phillips also didn’t hold a NHA license, and like Kanaley, Phillips had no experience running a skilled nursing facility.
After conducting a 10-month nationwide search, Mr. Phillips was hired in April 2020 to replace Hirose. Phillips had most recently served as CEO of the Silver Lake Medical Center in Los Angeles for one year and 11 months. Silver Lake Medical Center is comprised of a dual-site 234-bed acute care Medical Center, including a 118-bed LPS Designated Behavioral Health Unit in the San Gabriel Valley and a 116-bed acute care hospital in downtown Los Angeles.
Knowledgeable observers suspect Phillips was hired at LHH based on his behavioral health unit experience, which could have come in handy with LHH’s increasing behavioral health patient mix, and the stain-inducing flow project. He served as LHH’s CEO for barely over two years, just after CMS yanked LHH’s CMS certification, leaving LHH facing the task of having to discharge up to 686 LHH patients, and the potential loss of close to $200 million annually in CMS reimbursement.
Phillips was the first LHH CEO to fail passing CMS surveys and re-survey’s that resulted in LHH losing CMS certification and reimbursement. He left LHH abruptly on June 2, 2022, probably involuntarily.
In the end, LHH has gone for the past 17 years without a licensed NHA, ever since Funk was deposed by Kanaley courtesy of the esteemed Mitchell Katz, and his replacements, first Barbara Garcia in 2011 after Katz was forced out in 2010, and then Dr. Grant Colfax who became Garcia’s replacement in February 2019.
Notably in the combined 21 years Funk, Kanaley, and Hirose served as LHH’s CEO, the hospital always retained its CMS certification and CMS reimbursement. It was only under Phillips that LHH lost its CMS certification and revenue.
Change Pickens Announced on June 30: “CMS-Required” Bed Reduction
As Dr. Derek Kerr adroitly reported in his new article: “Karma or Persecution: Laguna Honda’s Ordeal” in the July 5 issue of the Westside Observer, Pickens'  claim on June 30 that the reduction of 120 beds was caused by the reduction of LHH’s three-person rooms to two-person rooms “ordered” by CMS is “intended to increase the quality of personalized care experiences.” That “order” may be pure hogwash, and may not actually be coming from CMS.
claim on June 30 that the reduction of 120 beds was caused by the reduction of LHH’s three-person rooms to two-person rooms “ordered” by CMS is “intended to increase the quality of personalized care experiences.” That “order” may be pure hogwash, and may not actually be coming from CMS.
Let me add to Dr. Kerr’s concerns by adding my own doubts.
First, Pickens offered no evidence or public records documenting that SFDPH had received any such recent “order” from either CMS or from California’s Department of Public Health. Indeed, of the seven CDPH inspection surveys conducted at LHH between October 14, 2021 and March 28, 2022 it is thought that there had been not one mention of, or deficiency issued, in the seven CDPH inspection reports regarding three-bedroom vs. two-bedroom Federal Tag (F-tag) violations of “personalized care experiences. And Pickens didn’t cite whether any such “order” had been received by LHH separate from, and in addition to, those seven inspections.
 Second, why would the architects designing the LHH replacement facility a few years before the new hospital and Patient Towers opened in 2010 have included three-person rooms, if that violated specifications for designing long-term care skilled nursing facilities?
Second, why would the architects designing the LHH replacement facility a few years before the new hospital and Patient Towers opened in 2010 have included three-person rooms, if that violated specifications for designing long-term care skilled nursing facilities?
Third, it was thought that both the two-person rooms and three-person rooms were designed and built at LHH were more like “suites,” perhaps containing a shared bathroom but with clear dividers, walls, and doors between each patients' bedrooms.
How can this suddenly be a new design requirement for long-term care skilled nursing facilities? How many other new SNF’s were constructed nationwide in the past 20 years that may also now be out-of-compliance with three-person rooms, and what will it cost to now reconfigure or convert those rooms nationwide to remain in compliance with CMS reimbursement rules?
 If there is magically and suddenly some new “current regulation” that Pickens is referring to that now requires only two-person rooms in new SNF construction projects, shouldn’t the new regulation have grandfathered in the existing three-person rooms constructed in earlier SNF construction projects?
If there is magically and suddenly some new “current regulation” that Pickens is referring to that now requires only two-person rooms in new SNF construction projects, shouldn’t the new regulation have grandfathered in the existing three-person rooms constructed in earlier SNF construction projects?
It’s embarrassing that LHH suddenly chose to delete 120 patient beds while simultaneously it added layers of Nursing management fat by adding the NHA and ANHA positions, probably at a combined cost of a minimum $400,00 between the two positions, given an LHH Associate Hospital Administrators earns about $160,000 (exclusive of benefits). By way of contrast in salaries, LHH’s Patient Flow Nurse Manager, Maria Chavez-Lagasca, earned $244,458 in the year ending June 2021, while Mr. Phillips earned $301,746, again exclusive of fringe benefits. It’s not known when SFDPH added a “Patient Flow Nurse Manager” to LHH’s staff it had had before.
 No money for beds, but plenty of money for salaries for nursing management “fat” salaries.
No money for beds, but plenty of money for salaries for nursing management “fat” salaries.
More Management Fat
The purpose of LHH’s two contracts with HMA and HSAG is premised on the need to improve: Executive Leadership, Organizational Structure, Medical Staff, Nursing Operations, Hospital Governing Body, and overall Management, among other issues.
It’s not known what “improvements” HMA thinks need to be made to LHH’s “Governing Body, since it is thought its Governing Body is the Health Commission, not SFGH. It’s not known if HMA was referring to changes to the “LHH-JCC” (a Health Commission subcommittee comprised of three Health Commission and senior management of LHH).
In addition to adding the new NHA and ANHA position, there are more named positions in the aggressive hiring plans.
HMA’s “preliminary assessment report” (which may have been “scrubbed” before SFDPH released it to members of the public), specifically states:
“The existing Laguna Honda nursing leadership structure did not provide sufficient resources and management bandwidth to effectively operate resident care units and support unit staff. HMA and Health Services Advisory Group (HSAG) jointly recommended an immediate modification to the nursing structure. One of the key changes recommended is to create three Director of Nursing (DON) positions. Two of the DONs would take responsibility for all units in a tower at Laguna Honda and would have a [single] Assistant Director of Nursing (ADON) reporting to each [DON]. In addition, a new DON position has been recommended to take responsibility for Nursing Operations, including services that are shared to support all units, such as Staffing, Education, etc.”
It's not known what SFDPH may have “cleaned” from HMA’s preliminary assessment report, given the report’s filename had included the word “cleaned” in the report’s filename.
 Pickens’ claim that LHH’s previous “nursing leadership structure did not provide sufficient resources and management bandwidth to effectively operate resident care units and support unit staff,” was preposterous and somewhat comical.
Pickens’ claim that LHH’s previous “nursing leadership structure did not provide sufficient resources and management bandwidth to effectively operate resident care units and support unit staff,” was preposterous and somewhat comical.
[Note: An extract of LHH’s pilot organization chart is available on my web site. The entire chart is too large to post on-line in a readable format because the fonts are so small. This extract of the org chart focuses on the bloated Nursing management structure. There’s only one way to spell senior Nursing management “bloat.”]
The org chart Pickens included in his June 30 letter to LHH staff announcing the elimination of 120 patient beds shows a total of 10 senior Nursing management employees, including: 1 Chief Nursing Officer (CNO), 1 Nursing Home Administrator (NHA), 1 Assistant Nursing Home Administrator (ANHA), 3 Directors of Nursing (DON), and 4 Assistant Directors of Nursing (ADON). Sounds to me like there will be at least seven, if not more, new hires. All of these positions starting at the DON management level report to LHH’s “Chief Nursing Officer” — who reports to LHH’s CEO.
Of the three new DON positions, one will be assigned to each of the two Patient Towers, and the third will be assigned to oversee Nursing Operations. The four new ADON’s will be split between the two Patient Towers, two to each Tower.
It looks to me like the Nursing Department’s “Nursing Operations” staffing is top-heavy with senior nursing staff who typically do not provide any direct patient care.
I think my friend, Virginia Leishman — who was the Director of Nursing at LHH for 43 years before retiring in 1997 — would have been appalled by the new bloated nursing management fat at LHH. She retired before I started employment there in 1999. I suspect that under her leadership LHH never failed to pass CMS inspection surveys or re-inspection surveys, and certainly never lost CMS certification or loss of CMS reimbursement during her four decades of service at LHH!
 In the decade I worked at LHH, preparations for CMS re-inspection surveys were always long and tense periods.
In the decade I worked at LHH, preparations for CMS re-inspection surveys were always long and tense periods.
Pickens’ org chart also shows 24 mid-level Nursing managers, including: 14 Nurse Managers and 10 Charge Nurses, but it doesn’t show an unknown number of Clinical Nurse Specialists overseeing various practice-area specialties who don’t provide direct patient care. All of this is before even getting to the RN’s, LVN’s, and CNA’s who actually do provide the day-to-day direct patient care.
Do similarly-sized SNF’s nationwide have similar levels of senior management fat as LHH’s pilot organization chart? Why not add 12 Drummers Drumming, 11 Pipers Piping, 10 Lords a Leaping, 9 Ladies Dancing, 8 Maids a Milking, 7 Swans a Swimming, 6 Geese a Laying, 5 Golden Rings, 4 Calling Birds, 3 French Hens, 2 Turtle Doves, and a Partridge in a Pear Tree, and an unknown number of additional catered lunches for nurses purloined from restricted Patient Gift Fund accounts?
 New Psych Tech Staff Additions
New Psych Tech Staff Additions
Remarkably, Pickens’ org chart shows that the North Tower ADON will indirectly supervise a Psych Tech, and the South Tower ADON will also indirectly supervise a second psych tech.
This is remarkable, because in 2010 (or earlier) LHH’s single Psych Tech position was eliminated in a SFDPH-wide a budget-cutting move. So, adding two Psych Tech backs onto LHH’s staff may be a step in the right direction and an encouraging sign. Some observers question whether that may be insufficient. At around 4:24:24 on videotape of the Board of Supervisors Committee of the Whole hearing about the potential closure of LHH, Pickens noted that about 20% of LHH’s then 674 patients — approximately 135 residents — had behavioral health “needs.” Of note, Pickens didn’t mention whether or not those “needs” involve actual primary or secondary psychiatric diagnoses.
Also, during the June 14 Board of Supervisors hearing Supervisor Mandelman asked general questions about LHH’s locked units (4:25:29 on tape). For her part, Supervisor Melgar stated definitively that “There are folks who are under conservatorship who need extensive care in locked facilities,” (at 4:25:29 on tape).
 While Melgar is undoubtably right that many people who are conserved do need to be in locked facilities, she may not have realized that Pickens was about to testify 30 minutes later (at 4:56:47 on tape) that the number of patients at LHH who have a public conservator is 101 people.
While Melgar is undoubtably right that many people who are conserved do need to be in locked facilities, she may not have realized that Pickens was about to testify 30 minutes later (at 4:56:47 on tape) that the number of patients at LHH who have a public conservator is 101 people.
DPH’s now required daily and weekly reports to CMS and California DPH have reported that there is a single “Locked/Secured Memory Care”unit only in the North Tower-Mezzanine unit, which SFDPH confirmed has only 60 beds. You can’t cram 101 people who may need to be in a locked (or secured) facility into a single LHH locked unit of just 60 beds.
It is also thought that LHH does not hold a psychiatric license to care for patients. Will just two Psych Techs be enough to help 135 behavioral health patients? Really?
It’s not known why Pickens suddenly implemented this pilot organizational restructuring and announced eliminating the 120 beds on June 30, just 6 days after the June 14 Board of Supervisor hearing, and just 23 days after the Health Commission had approved funding for the two contracts on June 7.
SFDPH Nurse Managers average $217,283, before fringe benefits. It sounds to me like the LHH Nursing Department new hires are going to cost well over $2 million annually in base pay and overtime alone, before fringe benefits. SFDPH had 16 Clinical Nurse Specialists (CNS) at the end of June 2021, who average $226,822 in base pay plus overtime (excluding fringe benefits). (The 16 CNS’s cost the City $3.63 million annually in salaries alone.)
All 16 may not work at LHH, (although LHH had several of them when I worked there). One of the 16 CNS — Mivic Hirose, who was let go as LHH’s CEO as a result of the patient sex abuse scandal in 2019 that cost the City a minimum of $1.8 million to date (with additional costs still climbing) — earned $265,686 in the year ending June 2021, including $29,000 in overtime, in a golden parachute position she landed in at SFDPH.
 My memory of the decade I worked at LHH is that there was a single DON (not three), and possibly a single ADON (not four), although there were plenty of unit Nurse Managers and Charge Nurses.
My memory of the decade I worked at LHH is that there was a single DON (not three), and possibly a single ADON (not four), although there were plenty of unit Nurse Managers and Charge Nurses.
Proximity in Time
Another issue involves the spatial proximity in time, which was remarkable — and highly suspicious.
 The two external consultants SFDPH hired to help LHH achieve CMS recertification — Health Management Associates (HMA) and Health Services Advisory Group (HSAG) — were awarded “emergency” no-bid contracts worth a combined total of $5,560,612. San Francisco’s Health Commission approved the two contracts on June 7, 2022. Additional costs continue to accrue.
The two external consultants SFDPH hired to help LHH achieve CMS recertification — Health Management Associates (HMA) and Health Services Advisory Group (HSAG) — were awarded “emergency” no-bid contracts worth a combined total of $5,560,612. San Francisco’s Health Commission approved the two contracts on June 7, 2022. Additional costs continue to accrue.
It was thought both consultants provided “preliminary assessment reports” of their initial recommendations on how to help ensure LHH gains CMS recertification were submitted to the DPH — which shared them with the Board of Supervisors by June 13, 2022. Only HMA’s “preliminary assessment report” has been made public.
Nothing to Hide? Sunshine Denied
In response to multiple records requests that have been placed to obtain HSAG’s “preliminary assessment report,” DPH first invoked a 14-day extension to produce the HSAG preliminary assessment report, citing the need to “consult with another interested City Department or agency” (most probably the City Attorney’s Office). Then on June 28, SFDPH changed it’s tune and claimed the HSAG preliminary assessment report is totally exempt under California’s Public Records Act and refused to provide the report, rather than just redacting parts of the report.
DPH has so far refused to provide any unredacted parts of HSAG’s preliminary assessment report.
What is in the HSAG preliminary assessment report the DPH is afraid of sharing with members of the public or LHH’s residents and their families? That opaque secrecy is the exact opposite of Pickens’ testimony to the Board of Supervisors on June 14 that SFDPH’s “goal is to be transparent. We have nothing to hide.”
The proximal period of time between the HMA “preliminary assessment report” that had been shared with the Board of Supervisors on June 13 and Pickens June 30 letter seven days later to LHH staff has raised concerns among knowledgeable observers about whether it may have been HSAG — rather than CMS — that asserted the nonsense about the new three-room rule regulation suddenly becoming a point of contention and used to justify and recommend LHH eliminate those 120 SNF beds at LHH..
This is a germane issue that should justify the Board of Supervisors rapidly scheduling a second hearing before the end of July before Board’s Government Audit and Oversight Committee that Supervisor Aaron Pekin had called for.
Such a hearing should be held before the end of July, and not be postponed to another Board of Supervisors Committee of the Whole hearing now scheduled for September 13. Patients facing out of-county discharges should not have to wait another 10 weeks before a hearing is scheduled to take up the issue of the sudden and permanent elimination of 120 beds at LHH before they are gone forever.
Eliminating 120 SNF beds in a town already critically short of SNF beds forcing the elderly and disabled out-of-county is a really, really bad idea. The Board of Supervisors need to step in, and intervene to stop this and probe for answers.
Here’s bottom line for the Board of Supervisors: Stop the premature discharges! Stop the bed cuts!
_____________________________________
Dedication: This article is dedicated to Larry Funk, who after he removal as LHH’s CEO but retained on staff to oversee completion of LHH’s rebuild in 2010, had privately and quietly encouraged me to continue my efforts to try to stop the downsizing of LHH by cutting 420 SNF beds. Funk stood in stark contrast to my boss, Dr. Lisa Pasqual, who was under enormous pressure from then Mitch Katz and John Kanaley to get me to shut up. Pascual had frequently flown into my office, slammed the door shut, and then shouted at me “Can’t you please tone down your Westside Observer articles?” To which I always replied by counting on my fingers: “1) I write my articles after hours and off the clock, 2) I value my First Amendment protections, and 3) The answer is ‘No, Lisa, I am not going to ‘tone myself down’,” knowing I had long passed probation and couldn’t be fired for off-the job protected speech.
I think Mr. Funk, Ms. Leishman, and my other dear friend and former co-worker — Sister Miriam Walsh, LHH’s Director of Pastoral Care for nearly 30 years (who passed away in December 2009 ) — would want all of us to continue fighting to stop the cut of another120 beds at LHH.
Monette-Shaw is a columnist for San Francisco’s Westside Observer newspaper, and a retired City employee. He received a James Madison Freedom of Information Award in the “Advocacy” category from the Society of Professional Journalists–Northern California Chapter in 2012. He’s a member of the California First Amendment Coalition (FAC) and the ACLU. Contact him at monette-shaw@westsideobserver.com.