 Printer-friendly PDF file
Printer-friendly PDF fileMay 12, 2023
Part 2: Qualitative Analysis of LHH’s
“Root Cause” Problems
Pre-Mortem of a Hospital:
One-Year Anniversary
‘Those Who Forget History Are Condemned to Repeat It’ Is Apropos
Laguna Honda’s Recurring Lack of Succession Planning May Well Repeat
by Patrick Monette-Shaw
As a reminder, April 14, 2023 was the first anniversary of LHH’s decertification. LHH claims it will apply for CMS recertification potentially by September 2023. That’s extremely doubtful.
Despite three consulting firms now having been on site at LHH for nearly a full year helping LHH correct its deficiencies, the status of the hospital remains unclear. Risks for obtaining its recertification remain — not fully abated.
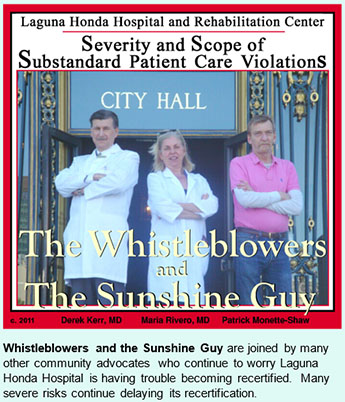
 As I indicated in my March 31 article, Doctors Derek Kerr and Maria Rivero published a terrific article on February 23 in the Westside Observer summarizing a portion of the qualitative root causes that led to LHH’s decertification that appeared in the first “Root Cause Analysis” (RCA) report San Francisco’s Department of Public Health had succeeded at keeping secret for nine weeks after it was submitted to CMS on December 1. The first RCA report was released on February 8, along with the second RCA report dated January 31 that was also submitted to CMS. Their article is a must read for anyone interested in the fate of LHH and its dwindling resident population. As of April 22, 2023 LHH’s census dropped to just 530 residents, compared to 710 residents on October 14, 2021.
As I indicated in my March 31 article, Doctors Derek Kerr and Maria Rivero published a terrific article on February 23 in the Westside Observer summarizing a portion of the qualitative root causes that led to LHH’s decertification that appeared in the first “Root Cause Analysis” (RCA) report San Francisco’s Department of Public Health had succeeded at keeping secret for nine weeks after it was submitted to CMS on December 1. The first RCA report was released on February 8, along with the second RCA report dated January 31 that was also submitted to CMS. Their article is a must read for anyone interested in the fate of LHH and its dwindling resident population. As of April 22, 2023 LHH’s census dropped to just 530 residents, compared to 710 residents on October 14, 2021.
Kerr’s and Rivero’s February article covered the first 48-page RCA Report prepared by Health Services Advisory Group (HAG), a consultant that has been paid $17.3 million to date to assist LHH obtain re-certification from CMS.
Their February article explored five of the first eight overarching problem categories in the first RCA report exploring the causal root factors leading to LHH’s decertification on April 14, 2022. Their article didn’t report on Categories 4, 5, and 8.
A caption to an illustration in their article asserted the first RCA gave readers a complete picture of LHH's problems.
 In my own article on March 31, I focused on the massive mound of quantitative data of the past three-year history of LHH’s citations for deficiencies uncovered during survey inspections by the California Department of Public Health (CDPH) on behalf of CMS.
In my own article on March 31, I focused on the massive mound of quantitative data of the past three-year history of LHH’s citations for deficiencies uncovered during survey inspections by the California Department of Public Health (CDPH) on behalf of CMS.
I take slight issue with saying the two RCA reports gave us a complete picture of LHH's problems. Even though LHH’s consultants have now released three monthly follow-up Monitoring Reports assessing LHH’s progress, I still believe we may not yet know the complete picture of what transpired at LHH. In fact, because LHH received substantial additional substandard care deficiencies following its second 90-Day Monitoring Survey report that ended in mid-March, more details of the complete picture are still dripping out, like a leaky faucet. The Quality Improvement Expert’s (QIE) fourth monthly “Monitoring Report,” and the third RCA report with additional “milestone” corrective actions, haven’t been released to the public yet. The third 90-Day Monitoring Survey is scheduled to start in late May or June.
It was shocking to learn the 63 detailed root causes uncovered that require 451 corrective actions to resolve 138 citations LHH has received. LHH had violated 78 separate patient care-related “F-Tags” — many multiple times each — plus an additional 20 “K-Tag” violations of facility “physical plant” deficiencies across the three years and four months since the sexual abuse of patients scandal at LHH surfaced in 2019. The 98 various types of “Tag” deficiencies led to the 138 citations documented in State inspection survey reports between July 2019 and November 2022.
 This article returns to reviewing more qualitative narrative culled from the two RCA reports released so far. LHH’s residents also deserve to have this qualitative information preserved for historical reasons, along with the quantitative analysis from my first article in this series. And preserved. LHH’s residents deserve to be cared for safely, without repeats of the many problems described below.
This article returns to reviewing more qualitative narrative culled from the two RCA reports released so far. LHH’s residents also deserve to have this qualitative information preserved for historical reasons, along with the quantitative analysis from my first article in this series. And preserved. LHH’s residents deserve to be cared for safely, without repeats of the many problems described below.
More on LHH’s Institutional Comorbidities
A second 90-Day Monitoring Survey that began on March 13 planned to take a week and conclude on March 17, 2023 will be followed by a third RCA report and a third additional “Action Plan” hasn’t been released yet. It’s overdue by weeks.
 In addition, as of May 12 there’s been a delay releasing the third part of inspection Form 2567’s from the second Monitoring Survey, so we don’t know all of the problems uncovered yet during that second survey. Nor have we seen how many more additional Action Plan “milestones” will be required in addition to the initial 451 corrective actions now underway. So, I’m very hesitant to conclude we have seen a complete picture of LHH’s problems that were decades long in the making.
In addition, as of May 12 there’s been a delay releasing the third part of inspection Form 2567’s from the second Monitoring Survey, so we don’t know all of the problems uncovered yet during that second survey. Nor have we seen how many more additional Action Plan “milestones” will be required in addition to the initial 451 corrective actions now underway. So, I’m very hesitant to conclude we have seen a complete picture of LHH’s problems that were decades long in the making.
The first RCA report asserted “The QIE identified and defined problems, investigated and collected supporting information specific to 21 survey citations, and analyzed and identified the root cause of each identified problem. The RCA specifically addressed deficiencies identified during surveys between October 14, 2021, and April 13, 2022, and all deficiencies that were discovered and disclosed to LHH by the California Department of Public Health (CDPH), CMS, or a contract surveyor after those surveys.”
One problem is that the QIE never identified the sources of documents it may have been provided and had reviewed after the April 13, 2022 CDPH Form 2567 inspection survey report. So, the public has no idea of what other deficiencies had been discovered at LHH. They may have been disclosed to LHH, but haven’t been disclosed to members of the public.
 HSAG, as the QIE, explained further that “The [RCA] report is organized by the eight foundational root cause categories that represent the systems-level areas needing significant improvement for LHH to sustain long-term compliance.” The first eight categories were:
HSAG, as the QIE, explained further that “The [RCA] report is organized by the eight foundational root cause categories that represent the systems-level areas needing significant improvement for LHH to sustain long-term compliance.” The first eight categories were:
1. Quality Assurance & Performance Improvement (QAPI)
2. Infection Prevention and Control
3. Behavioral Health and Substance Abuse
4. Medication Management and Administration
5. Resident Rights and Freedom from Harm
6. Comprehensive Care Plans and Quality of Care
7. Competent Staff, Training, and Quality of Care
8. Emergency Preparedness Program
Let’s start by reviewing the other three main categories Kerr and Rivero hadn’t discussed.
The First “Root Cause Analysis” Report
The first “Root Cause Analysis” report had identified three additional main categories of problems, including:
4. Medication Management and Administration
The consultant’s uncovered four separate “root causes” in this category alone.
The “problem statement” for this category issued a damning assessment, saying “LHH medication management and administration policies are inconsistently applied, resulting in resident medication safety issues and non-compliance with Federal regulations.”
 The report went on to assert: “LHH licensed nursing staff are not compliant with medication management policies and procedures, such as managing the safe storage of medications, disposing of medications appropriately, checking expiration dates on medications, and securing medication carts. This results in non-compliance with safe storage and disposal of drugs and biologicals.”
The report went on to assert: “LHH licensed nursing staff are not compliant with medication management policies and procedures, such as managing the safe storage of medications, disposing of medications appropriately, checking expiration dates on medications, and securing medication carts. This results in non-compliance with safe storage and disposal of drugs and biologicals.”
The high-priced consultant’s claimed “LHH pharmacy and nursing leadership will collaborate to develop a program that regularly validates effective medication management that includes safe storage, accurate labeling, appropriate medication disposal, and checking expiration dates.” This should have been standard operating procedure, all along. How it became a major issue is worrisome, but a sign of just how far out of regulatory compliance LHH’s lax nursing staff had become.
5. Resident Rights and Freedom From Harm
 The consultant’s uncovered another eight “root causes” in this category alone.
The consultant’s uncovered another eight “root causes” in this category alone.
The “problem statement” for this category revealed other concerning issues, saying “LHH daily operations have several characteristics that limit a holistic focus on residents’ well-being … [including] limited resident-centered care practices … poorly implemented interventions after abuse allegations … lack of consistent leadership, and [lack of] management oversight to ensure residents rights are consistently met.”
What a mouthful!
Among the eight root causes, one of the worst, from my perspective, is Root Cause 5: “LHH staff have not fully embraced resident-centered, evidence-based concepts, such as consistent nursing assignment, hourly rounding, or no-pass zones, resulting in a lack of awareness of resident needs, a clean and safe homelike environment, and prolonged response to call lights. This increases the likelihood of a decrease in quality of life and a dignified existence for residents.”
 Just as troubling is Root Cause 6: Lack of strong accountability standards. The consultant’s asserted: “Organizational accountability does not include progressive disciplinary action for consistent, documented, non-compliant staff behaviors affecting resident rights and dignity.” Wow! No accountability for staff screw-ups? No disciplinary action to weed out staff transgressors? Has that been a problem, all along?
Just as troubling is Root Cause 6: Lack of strong accountability standards. The consultant’s asserted: “Organizational accountability does not include progressive disciplinary action for consistent, documented, non-compliant staff behaviors affecting resident rights and dignity.” Wow! No accountability for staff screw-ups? No disciplinary action to weed out staff transgressors? Has that been a problem, all along?
Another shocker was Root Case #8: Lack of a formalized restorative nursing program. The consultant revealed: “LHH does not have a formalized restorative nursing program with defined ownership. The current process is not designed to maintain the functional ability of residents, resulting in inconsistent assessments for mobility and care planning and poor implementation of specific interventions. This increases the likelihood that residents could be at increased risk for harm due to declines in range of motion, mobility, and quality of life.”
As a reminder, back in1998 the U.S. Department of Justice had launched an investigation into LHH’s failures to prevent its patient’s further functional decline by not providing adequate physical therapy, occupational therapy, and speech-language pathology “restorative” therapeutic services. LHH had developed two Restorative Care program components, which LHH’s current administration had allowed to slip into decline (again). It’s a wonder the U.S. DoJ hasn’t come knocking on LHH’s door again, although it remains a concern of CMS under Xavier Becerra’s leadership at the U.S. Department of Health and Human Services (DHHS). Perhaps LHH’s Jennifer Carton-Wade — initially an Occupational Therapist who climbed through the ranks to become a current “Administrative Director” in LHH’s “C-Suite” — can explain (but hasn’t to date) why she allowed LHH’s Restorative Care Program to go missing in action again in 2014 under her “leadership” in LHH’s Rehabilitation Services Therapy department.
8. Emergency Preparedness Program (EPP)
The last category in the first “Root Cause Analysis” report prepared by the consultant’s included six more “root causes” in this category.
The consultant’s problem statement indicated “LHH’s EPP does not have elements in place, such as readily available emergency information, resulting in an ineffective program that lacks standardization across the facility. LHH also has gaps in regular training and exercises, contributing to an EPP that is out of compliance with Federal emergency preparedness requirements.”
 Shockingly, Root Case #6 in this category concluded: “Residents and resident representatives are unaware of their responsibilities as outlined in the emergency plan, which is not provided to them at the time of admission, nor are they included in EPP exercises, resulting in residents and visitors not being prepared during an emergency. This increases the likelihood of harm.”
Shockingly, Root Case #6 in this category concluded: “Residents and resident representatives are unaware of their responsibilities as outlined in the emergency plan, which is not provided to them at the time of admission, nor are they included in EPP exercises, resulting in residents and visitors not being prepared during an emergency. This increases the likelihood of harm.”
Excluding residents from emergency preparation drills also seems to run counter to LHH’s decades long claim of “residents come first.”
 The additional three problem categories discussed above are just as alarming, and just as damning!
The additional three problem categories discussed above are just as alarming, and just as damning!
As Kerr and Rivero had reported, the sixth category involving “Comprehensive Care Plans and Quality of Care” had asserted:
“Resident care plans are not individualized and are not being used effectively as an accessible tool for the [Interdisciplinary Care Teams] to plan and document care and accomplish individualized care goals … and overall quality of life for residents. This results in LHH not delivering care that meets professional standards of quality. This leads to poor resident outcomes in areas such as accident hazards, respiratory care, pain management, dietary needs, and range of motion.”
Becerra, DHHS, CMS, and CDPH are rightly concerned about the substandard quality of care provided at LHH. DHHS and CMS arerequired to make sure that LHH’s patients are cared for safelyand with the care that they're supposed to have. They have no choice by law and Federal regulations but to say the safety of LHH’s patients must come first. That’s why they’re trying to get LHH back into substantial compliance with CMS’ regulations. That’s what CMS is supposed to do!
The Second “Root Cause Analysis” Report
Two months after the first Root Case Analysis report dated December 1, 2022 was submitted to CMS, LHH’s QIE wrote a second Root Cause Analysis report dated January 31 based on the first “90-Day Monitoring Survey” that was conducted and completed at LHH in December. The second RCA report uncovered three additional foundational root cause categoriesneeding significant improvement at LHH, presented below.
9. Fire and Life Safety
The consultant’s problem statement indicated “LHH fails to fully follow the Fire and Life Safety (FLS) code throughout the facility, which could lead to an unsafe environment for residents and staff. … LHH staff fail to recognize and report out-of-compliance safety issues. This was evidenced in the [first 90-Day] monitoring survey with 21 K-tag findings, including, but not limited to, means of egress, fire alarm control functions, sprinkler systems, elevators, and electrical equipment.”
 The report listed by name and number only 20 of the 21 K-Tag citations (creatively mischaracterized as mere “findings”),
The report listed by name and number only 20 of the 21 K-Tag citations (creatively mischaracterized as mere “findings”),
suggesting one of the 20 specific Tag numbers may have been cited twice for separate incidents.
The consultant’s further noted that Root Cause #3 in this category, Lack of code compliance knowledge that “The LHH Facilities Department lacks thorough regulatory and code compliance knowledge, resulting in a limited ability to proactively identify potential life safety issues. This increases the risk that important issues are not fixed in a timely manner.” Isn’t knowledge of code compliance regulations a prerequisite for jobs in the Facility Services Department?
Root Cause #4 in this category, Ineffective preventative maintenance program reported “LHH does not have a formal preventative maintenance program, resulting in a lack of proactive, consistent maintenance on equipment throughout the facility. This increases the risk that equipment may break or be out of service.”
For instance, elevators have often been out of service for long periods of time, even though the building is just 13 years old.
Another grave concern is, how can a facility of this size and importance not have had a formal schedule for, and actively monitored, preventative maintenance programs? This is a sure sign of gross mismanagement. Does that happen at SFGH, affecting acute-care hospital patients, too?
10. Resident Quality of Care
As if the three categories of Infection Prevention and Control, Resident Rights and Freedom from Harm, and Comprehensive Care Plans and Quality of Care uncovered in the first RCA report weren’t alarming enough, along came the new category of Resident Quality of Care uncovered during the second RCA report.
 The consultant’s problem statement for this category reported “LHH does not adequately maintain programs with monitoring, training, and feedback mechanisms to ensure consistent resident quality of care. This was evidenced in the [first 90-Day] monitoring survey that identified that LHH lacked an effective wound management program that meets … the nutritional needs of residents and ensures proper positioning of residents … which could result in actual harm. In addition, the survey identified inconsistent practices for residents in need of tube feeding and pain management practices.”
The consultant’s problem statement for this category reported “LHH does not adequately maintain programs with monitoring, training, and feedback mechanisms to ensure consistent resident quality of care. This was evidenced in the [first 90-Day] monitoring survey that identified that LHH lacked an effective wound management program that meets … the nutritional needs of residents and ensures proper positioning of residents … which could result in actual harm. In addition, the survey identified inconsistent practices for residents in need of tube feeding and pain management practices.”
In fact, the consultant reported State surveyors had cited LHH for 14 F-Tag violations in the Resident Quality of Care category alone during the first 90-Day Monitoring Survey, including three of five “G” Severity and Scope violations during the entire survey. “G” citations represent isolated “Actual Harm” violations that don’t rise to the level of “Immediate Jeopardy.”
 The consultant shoehorned the 14 violations into four Root Causes for this category, including Root Cause #1, Lack of a functioning wound care program,” noting “LHH leadership did not ensure the wound care program continued to function appropriately after the retirement of a wound care nurse, resulting in a lack of individualized interventions being put into place. This worsened resident wounds and increased the risk of actual harm to the resident.”
The consultant shoehorned the 14 violations into four Root Causes for this category, including Root Cause #1, Lack of a functioning wound care program,” noting “LHH leadership did not ensure the wound care program continued to function appropriately after the retirement of a wound care nurse, resulting in a lack of individualized interventions being put into place. This worsened resident wounds and increased the risk of actual harm to the resident.”
The consultant’s recommendation was that “LHH … develop and implement an effective wound care program” and asserted that LHH, through its QAPI (Quality Assessment and Performance Improvement) program’s governing body, “will also create a process to ensure the wound care program can continue during staff turnover.”
Duh! Isn’t succession planning to continue programs when an existing staff member departs a routine practice at LHH? The answer may be “No,” because when the prior leaders of LHH’s separate “Restorative Care Nursing” program had staff turnover, that program also bit the dust due to poor succession planning. Same problem, different program.
Worse, the consultant reported Root Cause #4, Inconsistent resident pain assessment documentation found that “Documentation of pain management is not consistently present in the EHR [Electronic Health Record system named “Epic”]. This results in a lack of consistent evidence of resident pain assessments before and after prn [medication not actually scheduled, and taken “as needed”] pain medication administration and before routine pain medication. This increases the risk that resident pain is not properly managed through individualized care plans.”
The failures of many modules in the Epic database cited repeatedly in the first two RCA reports have contributed heavily to many other deficiencies that caused LHH’s decertification. Epic was not initially designed for managing electronic medical records of skilled nursing facility residents. It was purchased for SFGH acute care patients, and shoehorned into tracking Laguna Honda patients’ medical records.
 After all, in Category 6, Comprehensive Care Plans and Quality of Care in the first RCA report, the consultant’s had identified Root Cause #5, EHR not optimized for SNF setting and lack of [Staff] EHR knowledge, saying “The Epic EHR utilized is not customized for the SNF setting and staff have limited knowledge of full EHR capabilities. This results in increased burden to staff to update and modify care plans, which increases the likelihood that residents have care plans with generic, acute-care–based interventions rather than comprehensive, resident-centered care plans.”
After all, in Category 6, Comprehensive Care Plans and Quality of Care in the first RCA report, the consultant’s had identified Root Cause #5, EHR not optimized for SNF setting and lack of [Staff] EHR knowledge, saying “The Epic EHR utilized is not customized for the SNF setting and staff have limited knowledge of full EHR capabilities. This results in increased burden to staff to update and modify care plans, which increases the likelihood that residents have care plans with generic, acute-care–based interventions rather than comprehensive, resident-centered care plans.”
No wonder the failures of LHH’s care plans have remained a continuing problem, and of continuing concern to CMS and CDPH!
It’s obvious the Epic database SFDPH rolled out in August 2019, including at LHH, has contributed significantly to many of the deficiencies and citations that led to LHH’s decertification in April of 2022 three years after Epic was purchased and implemented. What a profound “original sin”!
11. Food and Nutrition Services
 The consultant’s problem statement for this category said “The LHH Food and Nutrition Services (FNS) program lacks consistency in documenting residents’ nutritional intake in the EHR [the Electronic Health Record database “Epic”], resulting in failure to properly assess intake adequacy and to follow through with treatment plans. In addition, LHH’s menu management system is not routinely monitored to ensure residents receive the correct meals, as prescribed. Furthermore, LHH lacks a systemic approach to monitor weight variance and wound status and to assess intervention effectiveness. This places residents at risk for not having their nutritional needs met and other adverse outcomes.”
The consultant’s problem statement for this category said “The LHH Food and Nutrition Services (FNS) program lacks consistency in documenting residents’ nutritional intake in the EHR [the Electronic Health Record database “Epic”], resulting in failure to properly assess intake adequacy and to follow through with treatment plans. In addition, LHH’s menu management system is not routinely monitored to ensure residents receive the correct meals, as prescribed. Furthermore, LHH lacks a systemic approach to monitor weight variance and wound status and to assess intervention effectiveness. This places residents at risk for not having their nutritional needs met and other adverse outcomes.”
The admission LHH’s menu management system and staff weren’t ensuring residents received their correct meals is alarming. Isn’t this basic for a skilled nursing facility seeking recertification?
The consultant squeezed the three F-Tag violations into four root causes for this category, including Root Cause #1 Menu management system not routinely verified, stating “LHH’s FNS [the Food and Nutrition Services Department] does not have a system in place to routinely update and verify information in its menu management system, resulting in incorrect nutrient analysis of menus served and missing food items. This increases the risk that residents do not receive meals based on their prescribed dietary order to promote optimal health and safety.”
Of the three F-Tag violations in this category, one included F692, Nutrition/Hydration Status Maintenance, assessed as a “G” citation representing isolated “Actual Harm” violations that don’t rise to the level of “Immediate Jeopardy.”
The consultant recommended LHH identify an on-site menu management system “superuser” to manage the menu management system and conduct routine quality assurance audits, and create a process to include reviews of menu item accuracy for quality assurance.
According to former LHH staff, the FNS department had developed processes even before 2010 to test meal-tray ticket items to ensure the proper diet textures, diabetic diets, and other dietary preferences were being correctly delivered to specific patients. Unfortunately, their disguised processes to test menu tray accuracy was discovered, rendering it somewhat useless, when not challenging to maintain their quality assurance process checks and balances.
 As for Root Cause #3, Lack of EHR knowledge and inconsistent data-entry practices, in this category the consultants reported “LHH’s Epic “EHR system is not fully configured for the SNF setting and staff lack EHR knowledge, creating challenges in [consistently] completing accurate documentation. This results in incomplete nursing documentation (with missing data entry on oral diet, snack, and supplement intake), decreasing clinicians’ ability to conduct accurate assessments due to the lack of essential resident information.”
As for Root Cause #3, Lack of EHR knowledge and inconsistent data-entry practices, in this category the consultants reported “LHH’s Epic “EHR system is not fully configured for the SNF setting and staff lack EHR knowledge, creating challenges in [consistently] completing accurate documentation. This results in incomplete nursing documentation (with missing data entry on oral diet, snack, and supplement intake), decreasing clinicians’ ability to conduct accurate assessments due to the lack of essential resident information.”
The consultants were referring, in part, to the failure of Nursing staff to document estimates of food and nutrition intake in patients’ medical records to assist nutritionist’s and registered dietitian’s collaboration during Interdisciplinary (Care) Team meetings (IDT). The consultants had reported “The LHH staff reported that the Food and Nutrition Services (FNS) program lacked consistency in documenting residents’ nutritional intake in the electronic health record (EHR).” That appears to be misplaced blame.
Dietitian’s are trained in medical nutrition therapies, but Nursing staff frequently assist patients eat during meals. Shouldn’t Certified Nursing Assistants (CNA’s) or other Nursing aide staff assisting patients during meals be documenting this in the medical records? This problem is addressed in more detail below.
 The dietary intake problems in Category 11, Food and Nutrition Services are related more to the Nursing Department failures than the FNS Department’s failures, but the consultants chose not to wade into additional criticisms of the Nursing staff. That said, there are admittedly problems with the third-party food menu management software LHH contracts with from the CBORD corporation. The consultant had claimed “LHH staff reported that the Food and Nutrition Services (FNS) program lacked consistency in documenting residents’ nutritional intake in the electronic health record (EHR).” But it seems clear the EHR documentation should have been performed by Nursing, not Food and Nutrition, staff.
The dietary intake problems in Category 11, Food and Nutrition Services are related more to the Nursing Department failures than the FNS Department’s failures, but the consultants chose not to wade into additional criticisms of the Nursing staff. That said, there are admittedly problems with the third-party food menu management software LHH contracts with from the CBORD corporation. The consultant had claimed “LHH staff reported that the Food and Nutrition Services (FNS) program lacked consistency in documenting residents’ nutritional intake in the electronic health record (EHR).” But it seems clear the EHR documentation should have been performed by Nursing, not Food and Nutrition, staff.
Subsequent Monthly QIE “Monitoring Reports”
As part of its consulting contract to be LHH’s Quality Improvement Expert (QIE), the HASG consultant, are required to produce monthly “Monitoring Reports” by the 10th of each month reporting on LHH’s progress toward implementing corrective action “milestones” during the preceding month. Only the first Monitoring Report dated February10 for progress in January following submission of the first RCA report in December, the second Monitoring Report dated March 10 for progress in February, and the third Monitoring Report dated April 10 for progress in March, have been submitted to CMS and released to members of the public.
The fourth Monitoring Report dated May 10 reporting on progress during April may have been submitted to CMS, but it hasn’t been released to the public to assess progress to date, and we haven’t learned how many additional corrective actions may have been added to the 451 milestones in the Action Plan (a.k.a., “Plan of Correction”). Unfortunately, the third RCA report following the second “90-Day Monitoring Survey” also hasn’t been released.
All corrective actions were supposed to have been completed by May 13. Also, LHH is nearing the time frame of when its third “90-Day Monitoring Survey” that is scheduled for late May or June is just upon us, leaving little time for LHH to fix any additional corrective actions before State inspectors show up at LHH again.
What we do know from the first three monthly “Monitoring Reports” is this: Across all three reports, there were a total of 346 “deliverables” identified and tied to fix the 451 corrective action “milestones.” Examples of Action Plan deliverables include literature reviews, assessment reports, gap analysis studies, revised policies and procedures, committee meeting minutes, audit results, and training materials.
Of those first 346 deliverables, 120 — 34.7% — had not passed muster following the QIE’s review and needed to be revised and resubmitted for re-approval after content revisions, guidance, and required coaching by the QIE to meet the intent of the Action Plan.
 Of note, 23 — 54.8% — of the 42 deliverables for the Comprehensive Care Plans and Quality of Care category deliverables required revision and resubmission. The problems with individualized care plans not being developed has been a major problem all along, and continued in the third Monitoring Report for the March time frame. Similarly, 14 — 40% — of the 35 deliverables in the Resident Quality of Care category also required revisions and resubmission.
Of note, 23 — 54.8% — of the 42 deliverables for the Comprehensive Care Plans and Quality of Care category deliverables required revision and resubmission. The problems with individualized care plans not being developed has been a major problem all along, and continued in the third Monitoring Report for the March time frame. Similarly, 14 — 40% — of the 35 deliverables in the Resident Quality of Care category also required revisions and resubmission.
Common reasons for the revisions included: 1) Lack of specificity with the information provided, 2) Information provided wasn’t what had been requested, 3) Information provided wasn’t for the time period identified in the milestone, and 4) General inattention to details (documents not dated, lacking a title, or without track changes so revisions could be identified).
What that suggests is that LHH staff who had no prior experience working in skilled nursing facilities weren’t capable of recognizing the problems and understanding what they had been asked to do, and providing appropriate corrective actions without substantial additional coaching and training. That their “homework” assignments had to be corrected and resubmitted is sad. Sadder, apparently their supervisors hadn’t noticed before the homework was submitted. LHH’s QIE isn’t going to be around forever to keep correcting their homework, unless LHH keeps paying millions more in “subject-matter expert” consulting fees annually.
Restorative Care Program
 LHH’s restorative care program was critiqued in the second and third monthly Monitoring Reports. In March, the QIE reported “LHH updated the current restorative program by defining parameters and updating policies … to align with Federal regulations.” A month later in the April report, the QIE added for good measure “The restorative nursing program has been newly redefined, and activities must have robust oversight to sustain program integrity. This includes care plan reviews and restorative program outcomes.”
LHH’s restorative care program was critiqued in the second and third monthly Monitoring Reports. In March, the QIE reported “LHH updated the current restorative program by defining parameters and updating policies … to align with Federal regulations.” A month later in the April report, the QIE added for good measure “The restorative nursing program has been newly redefined, and activities must have robust oversight to sustain program integrity. This includes care plan reviews and restorative program outcomes.”
Gee, who would have thought to actually “monitor outcomes”? Ya’ think? What a concept — which should have been obvious! Belatedly suggesting the need for continuing “robust oversight” is a slap in the face to LHH’s residents. And it’s shocking the QIE consultants worry that without robust oversight the restorative program might not be sustained for long — again!
That failure to monitor post-discharge transfer outcomes last summer may have contributed to the 12 patient deaths due to transfer trauma following involuntary patient evictions resulting from LHH’s initial but flawed Closure Plan.
 All of this was ridiculous, because LHH had developed an award-winning Restorative Care Level I and Level II program components two decades ago in 1999 … but it was abandoned and lapsed in 2014. It’s unclear whether the QIE had even examined the Restorative Care Level I policy and procedure adopted 20 years ago, which had complied at the time with Federal regulations.
All of this was ridiculous, because LHH had developed an award-winning Restorative Care Level I and Level II program components two decades ago in 1999 … but it was abandoned and lapsed in 2014. It’s unclear whether the QIE had even examined the Restorative Care Level I policy and procedure adopted 20 years ago, which had complied at the time with Federal regulations.
Assessing Food and Nutrition Intake
 The third “Monitoring Report” noted that during the QIE’s interview with LHH’s Chief Clinical Dietitian on March 20, 2023, she was asked what challenges are occurring with the unit based QAPI Wounds and Nutrition committee meetings. The Chief Dietitian indicated “some [patient care] units are not obtaining weekly weights as ordered.” The QIE reported that the Director of Nursing (DoN, an HSAG consultant in an acting capacity) had also shared that during one of the Monitoring Surveys she was asked (potentially by a State surveyor), “How does staff know what a 50% meal intake looks like?”
The third “Monitoring Report” noted that during the QIE’s interview with LHH’s Chief Clinical Dietitian on March 20, 2023, she was asked what challenges are occurring with the unit based QAPI Wounds and Nutrition committee meetings. The Chief Dietitian indicated “some [patient care] units are not obtaining weekly weights as ordered.” The QIE reported that the Director of Nursing (DoN, an HSAG consultant in an acting capacity) had also shared that during one of the Monitoring Surveys she was asked (potentially by a State surveyor), “How does staff know what a 50% meal intake looks like?”
In reflecting on that, the DoN recognized “an opportunity to provide education to the Nursing department to improve the competencies of staff members, so they accurately record meal intake percentages.” This is being developed for an April 2023 training event, with instructors using a visual chart that shows partially-eaten meals and how that translates into percentages.
This is another big “Duh”! After all, this is a Nursing staff duty — as recognized by the DoN herself — since dietary and nutrition staff are typically not on the patient units during mealtimes. Why train Nursing staff on this if it isn’t in their job duties? Former LHH staff have reported that the same dietary chart illustrating meal intake percentages had been used as far back as a dozen years ago, if not earlier. Rather than just presenting it during a one-time training session, the chart should be posted on each of the 13 Nursing units — or better yet, in each patients’ rooms. There are a little over 300 patient suites, between two-person and three-person suites. And there’s only a handful of congregate patient  dining rooms. Surely, LHH can pay for reproduction of 300 wall signs to post in each residents’ suites to ease nutrition intake monitoring, assessment, and data collection, which should be monitored by CNA’s or other Nurse aides when meal trays are picked up.
dining rooms. Surely, LHH can pay for reproduction of 300 wall signs to post in each residents’ suites to ease nutrition intake monitoring, assessment, and data collection, which should be monitored by CNA’s or other Nurse aides when meal trays are picked up.
For a skilled nursing facility that claims its “residents come first,” LHH’s residents deserve no less.
Hire Competent Staff Having Previous Relevant Experience
Kerr and Rivero concluded their February article saying:
“The root cause of this debacle is the colonization of Laguna Honda Hospital by SF General [Hospital] via the DPH ‘Flow Project.’ Economics played a role. But hubris drove the deformation of LHH. The ‘best and the brightest’ from DPH and SFGH devalued long-term care for the elderly.
 Now, outside experts affirm that even LHH’s newly installed ‘leaders’ don’t know what they’re doing. It’s shameful that federal and state regulators had to force the DPH to redress the incompetence it rammed into LHH.”
Now, outside experts affirm that even LHH’s newly installed ‘leaders’ don’t know what they’re doing. It’s shameful that federal and state regulators had to force the DPH to redress the incompetence it rammed into LHH.”
That’s still true. Now 12 months after LHH was decertified in April 2022, it’s still unclear whether these leaders know what they are doing, despite hiring so-called outside “expert” consultants.
We can only hope that when LHH finally hires and “on-boards” a licensed Nursing Home Administrator as its CEO — which it hasn’t had for 20 years, since its last licensed NHA, Larry Funk, was forced out in 2004 — that history won’t repeat itself by not actively engaging in succession planning, and hiring and retaining LHH staff who are actually knowledgeable about — and have previous relevant experience with — substantial compliance with Federal nursing home regulations.
 Otherwise, LHH’s current debacle may well be doomed and condemned to a repeat, since as things now stand, LHH’s future has a poor prognosis.
Otherwise, LHH’s current debacle may well be doomed and condemned to a repeat, since as things now stand, LHH’s future has a poor prognosis.
If we forget this history, a repeat may be inevitable.
Monette-Shaw is a columnist for San Francisco’s Westside Observer newspaper, and a retired City employee. He received a James Madison Freedom of Information Award in the “Advocacy” category from the Society of Professional Journalists–Northern California Chapter in 2012. He’s a member of the California First Amendment Coalition (FAC) and the ACLU. Contact him at monette-shaw@westsideobserver.com.