 Printer-friendly PDF file
Printer-friendly PDF fileApril 22, 2024 Updated: May 26, 2024
Costs to Rescue Laguna Honda Hospital Soar to $125M $177.5 Million
LHH’s Decertification 2nd Anniversary Disaster
Will 120 of Laguna Honda Hospital’s Beds Be Eliminated?
Will There Be Patient “Cohorting”? When Will Admissions Restart?
Ignore Public Documents That Cost $40 Million as Just “Hearsay”
by Patrick Monette-Shaw
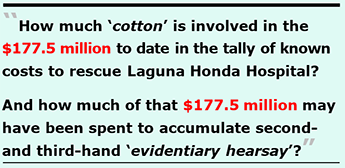
Traditional second anniversary gifts are made of cotton, because it symbolizes the strength, weave, and comfort between two parties.
Interestingly, paper U.S. currency is made of 25% linen and 75% cotton, with red and blue fibers distributed randomly throughout to make forgeries more difficult.
A reasonable question is how much cotton is involved in the $125 million $177.5 million to date in the running tally of known costs to rescue Laguna Honda Hospital? That much cotton would represent an enormous anniversary gift.
Another reasonable question is whether, and how much, of the$125 million $177.5 million may have essentially been spent to accumulate second- and third-hand “evidentiary hearsay”?
 Obviously, nobody wants to see our beloved Laguna Honda Hospital shut down because it is too expensive to save. But ever since LHH was decertified on April 14, 2022, and new admissions to LHH were instantly halted, it is almost as if the Board of Supervisors handed external consultants and San Francisco’s Department of Public Health (SFDPH) carte blanche using the City’s dime to spend however they saw fit.
Obviously, nobody wants to see our beloved Laguna Honda Hospital shut down because it is too expensive to save. But ever since LHH was decertified on April 14, 2022, and new admissions to LHH were instantly halted, it is almost as if the Board of Supervisors handed external consultants and San Francisco’s Department of Public Health (SFDPH) carte blanche using the City’s dime to spend however they saw fit.
When I first began to tally the associated costs to rescue Laguna Honda, there were four main categories, that started out totaling about $64.1 million on July 14, 2023. That grew 17 days later on July 31, 2023 to $64.9 million.
Rapidly, costs soared by at least another $39 million by September 15, 2023 that I have not written about since last August. Since mid-September, the running tally in documented expenses to rescue Laguna Honda have nearly doubled tripled from $64.9 million. The known costs to date have now crept up to at least $125 million $177.5 million — and counting — described in further detail in this article in an effort to preserve the historical record.
 Few other nursing facilities nationwide that get decertified like Laguna Honda Hospital was have the luxury of that level of spending to save a facility, and do not have the luxury of having municipal tax dollars to bail out a nursing home.
Few other nursing facilities nationwide that get decertified like Laguna Honda Hospital was have the luxury of that level of spending to save a facility, and do not have the luxury of having municipal tax dollars to bail out a nursing home.
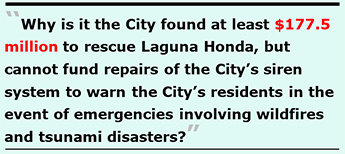
By way of comparison, San Francisco’s emergency warning siren system was shut down in December 2019 due to the possibility of electronic hacking of the system. Here we are four-½ years later and the $5 million to now $20 million needed to bring those sirens back on-line still has not happened! [The longer San Francisco waits, the higher the costs will be to replace the siren system.]
Following the wildfires that all but destroyed Lahaina on Maui on August 8, 2023 Board of Supervisors president Aaron Peskin indicated publicly he had identified funding to restore the siren system. Here we are eight months later, and Peskin has done nothing towards getting the siren system fully funded, but he found time to throw his hat into the ring to run to replace Mayor Breed in November’s election.
 Why is it that the City has found at least
Why is it that the City has found at least $125 million $177.5 million to rescue Laguna Honda, but cannot fund repairs of the City’s emergency siren system to warn the City’s 810,000 residents in the event of wildfires and tsunami disasters? Where has $125 million $177.5 million gone in just a two-year period? And why hasn’t that spending accomplished LHH’s re-certification by now?
Since this article was first published on April 22, the City’s Department of Public Health belatedly announced on May 21 a new $52.5 million shortfall in LHH’s Medi-Cal and Medicare revenue during the first three quarters of its current Fiscal Year 2023–2024 through March 31, 2024 now added into Table 1 below; that may increase in the fourth quarter.
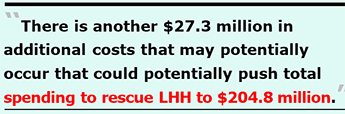
Public documents reveal the $125 million $177.5 million in known costs to date have grown from four major categories of spending to seven main categories, shown in Table 1 below (or on-line). Unfortunately, there is another $27.3 million in additional costs that may potentially occur shown on rows 8 and 9 9 and 10 in Table 1 that could potentially push total spending to rescue LHH to $152.3 million $204.8 million. Those two rows need brief explanations.
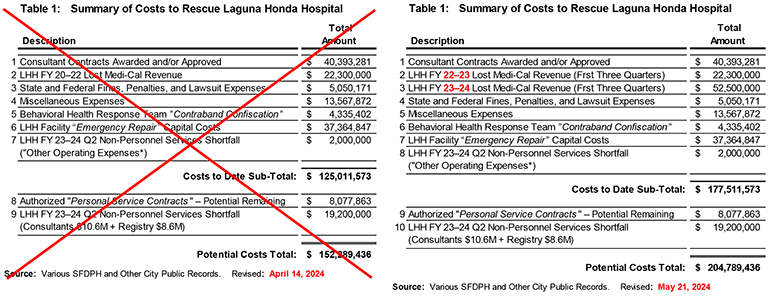
The $8 million on Line 9 in Table 1 is the remaining balance from $18 million authorized on Civil Service Contract #PSC 40941-22/23 approved by San Francisco’s Civil Service Commission on September 6 to hire external consultants to assist with the Laguna Honda recertification. SFDPH issued a fourth contract for $9.92 million to Health Services Advisory Group (HSAG) against that $18 million PSC authorization number, leaving a balance of just over $8 million. SFDPH could theoretically issue another consulting contract against that remaining authorization without having to seek further approval.
The $19.2 million of potential “non-personnel services” costs on Line 10 in Table 1 is a little murkier. On March 5, SFDPH’s Chief Financial Officer, Jenny Louie, presented SFDPH’s Second Quarter FY 2023–2024 Revenue and Expenditure Projection Report to the full Health Commission. Louie’s report noted LHH had a $21.2 million “Non-Personnel Services” revenue shortfall she attributed to being a “recertification-related expenditure deficit.”
A subsequent public records request revealed the $21.2 million “expenditure deficit”involved $10.6 million in recertification consulting and recertification training services contracts, $8.6 million in staffing “registry” costs, and $2 million in “other operating expenses” for things such as equipment rental and maintenance, and translation services. For purposes of tracking the actual running costs of LHH’s recertification expenses, the $2 million in “other operating expenses” has been added to Table 4, “Miscellaneous Expenses” below.
[Note: An additional $10.65 million in separate personnel staffing costs attributed to hiring temporary as-needed “registry” staff confirmed by responses to other public records requests are included in Table 2 and Table 4 below, distinct from and beyond the $8.6 million in registry costs included in the $19.2 million potential “expenditure deficit.”]
For the time being the remaining $19.2 million on Line 9 in Table 1 remains as a potential additional cost of getting Laguna Honda recertified. That’s because it isn’t clear whether the $19.2 million was actually eventually magically “realized,” or “amortized” and somehow balanced out after just being a temporary budgeting difference between anticipated funding sources that were eventually earned and only temporarily considered a shortfall or deficit. So they’re listed as potential costs in this running tally in case they are duplicate expenses included elsewhere in the known $125 million $177.5 million in costs.
Alternatively, it’s not clear if the $19.2 million in non-personnel services shortfall expenses were not included elsewhere in the accounting in this article and were not “resolved” in SFDPH’s budgeting gymnastics as having been covered by other surpluses and savings from other SFDPH budget areas that were pressed into service to pay for, resolve, and erase the “recertification-related expenditures” deficit to arrive at a balanced budget revenue and expense report. In other words, did the $19.2 million in non-personnel services expenses actually occur but had never been identified beforehand with an authorized budget allocation authorized explicitly for LHH’s recertification, and were simply paid for using other areas of SFDPH’s budget?
The $19.2 million in potential costs has been segregated from the actual known costs to date, because they potentially may or may not involve duplicate items elsewhere accounted for in other tables in this article. They may actually refer to excess spending above and beyond budgeted expenses. This would require the services of a forensic accountant to get SFDPH or the City to tell the truth about the total spending required to rescue Laguna Honda. I readily admit I am not an accountant.
Unfortunately, if the $27.3 million in additional potential costs on lies 9 and 10 come to pass, we’ll reach $152.3 million $204.8 million in spending to rescue Laguna Honda.
Whether mismanagement of LHH resulted in “only” $125 million $177.5 million or increases to $152.3 million $204.8 million in costs to save our beloved 150-year-old “alms house,” that suggests heads should continue to roll; additional senior management replacements still need to occur; and stronger and more meaningful oversight mechanisms must be implemented to correct the “governing body” oversight mechanisms in place that utterly failed to prevent Laguna Honda’s decertification two years ago.
Laguna Honda Hospital’s entire mismanagement fiasco and enormous associated expenses must never recur, ever again!
The Consultant Contracts
When LHH was decertified on April 14, 2022 San Francisco’s Department of Public Health (SFDPH) sprang into action and quickly issued three contracts to bring in outside consultants to help straighten out the18 year history of LHH’s mismanagement. The first three contracts started out at a relatively benign $9 million cost, shown in Table 2, below (or on-line). The consultants began work on May 9, about three weeks following LHH’s decertification.
By the end of 2022, the first three contracts had quickly grown to $16.3 million via contract amendments.
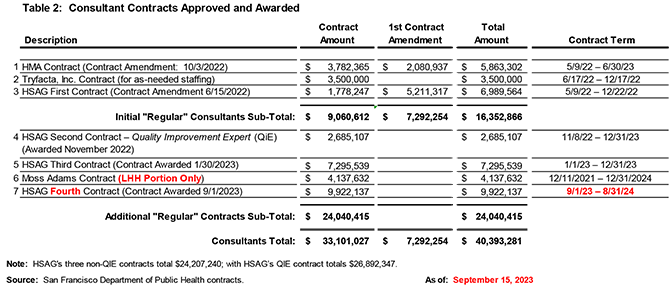
 Although I first reported on July 14, 2023 that in the first year following LHH’s decertification, SFDPH and LHH had issued $30.5 million hiring consultant to come in and help “fix” Laguna Honda, only two months later a fourth contract with Health Services Advisory Group (HSAG) was issued for $9.92 million (just under the $10 million threshold that would have sparked another Board of Supervisors hearing to approve HSAG’s fourth contract).
Although I first reported on July 14, 2023 that in the first year following LHH’s decertification, SFDPH and LHH had issued $30.5 million hiring consultant to come in and help “fix” Laguna Honda, only two months later a fourth contract with Health Services Advisory Group (HSAG) was issued for $9.92 million (just under the $10 million threshold that would have sparked another Board of Supervisors hearing to approve HSAG’s fourth contract).
That pushed contracts with external consultants to $40.4 million during the first 17 months following LHH’s decertification.
For some corroboration of the $40 million estimate awarded for consultants to date, a declaration filed by LHH’s Chief Quality Officer, Nawzaneen Tali, in a San Francisco Superior Court on March 18 in yet another lawsuit involving Laguna Honda acknowledges $28.8 million has already been paid to the consultants, with another $8 million in unpaid invoices waiting for payment, totalling approximately $36.8 million in consultant contracts to date. The $3.6 million difference to the full $40.4 million shown in Table 2 may well be invoiced in coming months for consulting work performed during the five-½ months between March 18 when Tali prepared her Declaration through the end of August. [After all, few contractors that latch on to lucrative City contracts forgo billing in full, not to sound jaded.]
It’s expected the $40.4 million amount will again increase, soon. That’s because Table 2 above shows HSAG’s fourth contract is set to expire just four months from now at the end of August. San Francisco’s Health Commission has already been forewarned HSAG’s contract will need to be extended for less-intensive assistance monitoring LHH’s compliance with CMS’ regulations after August 2024, whether or not LHH gains recertification by then and patient admissions actually resume.
 Of some interest, the main contractor — Health Services Advisory Group (HSAG) — has earned a total of $26.9 million in contracts. HSAG has been paid to produce approximately 507 pages of reports sent to CMS and the California Department of Public Health (CDPH). But shockingly, in a long drawn-out lawsuit against Laguna Honda Hospital, City Attorney David Chiu had the chutzpah to advise San Francisco’s Superior Court on March 18, 2024 to treat HSAG’s nine “Root Cause Analysis Reports,” seven monthly “Monitoring Reports,” and extensive “Action Plans” as merely double or triple hearsay.
Of some interest, the main contractor — Health Services Advisory Group (HSAG) — has earned a total of $26.9 million in contracts. HSAG has been paid to produce approximately 507 pages of reports sent to CMS and the California Department of Public Health (CDPH). But shockingly, in a long drawn-out lawsuit against Laguna Honda Hospital, City Attorney David Chiu had the chutzpah to advise San Francisco’s Superior Court on March 18, 2024 to treat HSAG’s nine “Root Cause Analysis Reports,” seven monthly “Monitoring Reports,” and extensive “Action Plans” as merely double or triple hearsay.
Why did the City pay $27 million to a contractor to develop 507 pages of mere “hearsay” evidence evaluating the causes of LHH’s mismanagement problems needing to be fixed? As unbelievable gall, can chutzpah be measured?
$22 Million $74.8 Million Lost Medi-Cal Revenue
As I first reported on July 14, 2023 SFDPH acknowledged in its May 12 Third Quarter Revenue and Expenditures report for Fiscal Year 2022–2023 (through March 31, 2023) that LHH had a $22.3 million loss in projected Medi-Cal revenue, given the halt on new admissions starting in April 2022, shown in Table 1 above.
The amount of lost Medi-Cal revenue has likely grown, but SFDPH has essentially buried that loss in subsequent quarterly revenue reports. Again, after this article was first published on April 22, San Francisco’s Department of Public Health belatedly announced a month later on May 21 a new $52.5 million shortfall in LHH’s Medi-Cal and Medicare revenue during the first three quarters of its current Fiscal Year 2023–2024 through March 31, 2024.
Averaging a loss of $17.5 million in each of those three quarters, it’s probably likely that during the fourth quarter of FY 2023–2024 LHH will incur the loss of an additional $17.5 million in foregone Medicare/Medi-Cal revenue — precisely because admissions to LHH are not likely to resume before June 30, 2024.
The loss of the Medicare/Medi-Cal revenue is highly problematic because LHH hasn’t reduced its staffing, despite having a 40.7% reduction in its patient population census since April 2022. Instead of paying for that staff using federal reimbursements, the salaries had to be made up from the City’s General Fund.
Combined, the lost revenue in FY 2022–2023 and FY 2023–2024 totals $74.8 million, excluding an unknown amount in the fourth qurter of FY 2022–2023 .
Back in May 2022, the City asserted LHH receives over $200 million a year in Federal reimbursement from Medi-Cal and Medicare when it is operating at full capacity. When LHH was decertified in April 2022, it was barred for admitting new patients. Just before it’s decertification, LHH had 710 residents on October 10, 2021, but since then its patient census has dropped to just 421 as of April 22, 2024 — a loss of 289 residents, representing a 40.7% change decrease.
Back in May 2022, the City asserted LHH receives over $200 million a year in Federal reimbursement from Medi-Cal and Medicare when it is operating at full capacity. When LHH was decertified in April 2022, it was barred for admitting new patients. Just before it’s decertification, LHH had 710 residents on October 10, 2021, but since then its patient census has dropped to just 421 as of April 22, 2024 — a loss of 289 residents, representing a 40.7% change decrease.
LHH has continued to receive Medi-Cal and Medicare reimbursement for the patients it still has. But given its reduction in residents to just 421, revenue from Medi-Cal has clearly declined, but it’s not known how much in total Medi-Cal revenue LHH has lost or may have otherwise earned.
 Logically, losing 40.7% of its patient population must have led to significantly more than just a $22 million decrease in Medi-Cal revenue. To the extent 95% of LHH’s residents relied on Medi-Cal as their payor source, losing 40.7% of $200 million translates to loss of over $77 million on an annual basis. (Although to be fair, the attrition of 289 patients has been spread over time, with a net loss of 163 residents in LHH’s first year of decertification, and the loss of the remaining 116 residents in the second year following decertification).
Logically, losing 40.7% of its patient population must have led to significantly more than just a $22 million decrease in Medi-Cal revenue. To the extent 95% of LHH’s residents relied on Medi-Cal as their payor source, losing 40.7% of $200 million translates to loss of over $77 million on an annual basis. (Although to be fair, the attrition of 289 patients has been spread over time, with a net loss of 163 residents in LHH’s first year of decertification, and the loss of the remaining 116 residents in the second year following decertification).
Obviously, Table 1 above seriously underestimates the total amount of lost Medi-Cal revenue at just $22 million $74.8 million. It’s likely far higher, whether SFDPH and LHH want to admit it, or not.
And while LHH’s patient population has dropped significantly, LHH’s operating expenses has not dropped by a corresponding level and have essentially remained constant. That’s because SFDPH and the City decided to keep LHH fully staffed, hoping to have resumed patient admissions long before now.
LHH has not only kept its full contingent of staffed employees, it actually had a 5.2% change increase in total employees, going from 1,422 Full-Time Equivalent (FTE) employees in March 2022 to 1,496 FTE’s as of March 29, 2024 — an effective increase of an additional 74 employees.
So while LHH’s revenues have dropped off, its operating expenses have increased significantly — an increased cost of doing business only partially captured by revenue losses outlined in this article.
Fines, Penalties, and Lawsuit Expenses
In my first report on July 14, 2023 and my second report on July 31, 2013 I reported that LHH’s fines, penalties and lawsuit expenses shown below in Table 3 had stood at $4,860,171.
But just a month later, San Francisco’s Board of Supervisors and the Mayor settled a case on August 31, 2023 awarding Andrew Coutts $190,000, increasing total fines, penalties and lawsuit expenses to slightly over $5 million shown in the updated Table 3 (or on-line).
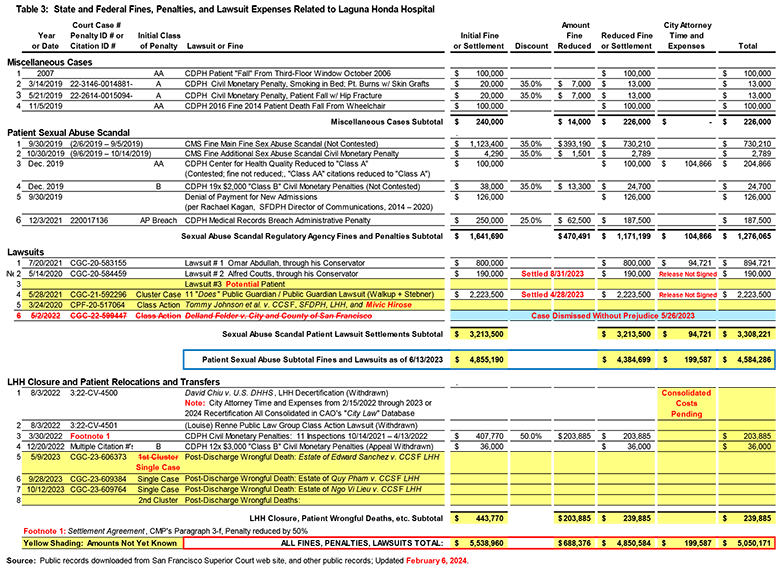
The total for Table 3 would be far higher than the $5 million shown, except that City Attorney David Chiu’s office is slow walking release of the costs of City Attorney time and expenses fighting the Coutts settlement and the Public Guardian / Public Conservator settlement shown on lines 2 and 4 in the “Lawsuits” section of Table 3. Chiu may be slow-walking release of his time and expenses data in those two cases as a legal strategy involving a third case involving the Tommy Thompson class action lawsuit which has not reached a settlement amount yet shown on Line 5 in the “Lawsuits” section.
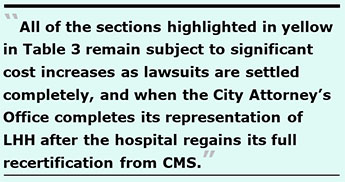 Importantly, all of the sections highlighted in yellow in Table 3 remain subject to significant cost increases as lawsuits are settled completely, and when the City Attorney’s Office (CAO) eventually completes its representation of LHH after the hospital regains its full recertification from CMS. That’s because the City Attorney has been providing highly-specialized on-going legal representation for two-½ years since at least October 2021, and the CAO’s legal services to prevent LHH from being closed completely has been accumulating in a single accounting code tracking money for the City Attorney’s multi-year time and expenses. The CAO more than likely won’t release its cumulative time and expenses for a year or two after LHH obtains its recertification, and the CAO closes out what is essentially a single multi-year billing account code.
Importantly, all of the sections highlighted in yellow in Table 3 remain subject to significant cost increases as lawsuits are settled completely, and when the City Attorney’s Office (CAO) eventually completes its representation of LHH after the hospital regains its full recertification from CMS. That’s because the City Attorney has been providing highly-specialized on-going legal representation for two-½ years since at least October 2021, and the CAO’s legal services to prevent LHH from being closed completely has been accumulating in a single accounting code tracking money for the City Attorney’s multi-year time and expenses. The CAO more than likely won’t release its cumulative time and expenses for a year or two after LHH obtains its recertification, and the CAO closes out what is essentially a single multi-year billing account code.
When that happens and the CAO stops representing LHH’s “decertification”-related nightmare, I predict the CAO’s time and expenses will be somewhere between an additional $10 million to $20 million, if not more — expenses that could have been avoided entirely had LHH simply stayed in substantial compliance with federal nursing home regulations and had never been decertified at all.
 Miscellaneous Projects and Staffing Expenses
Miscellaneous Projects and Staffing Expenses
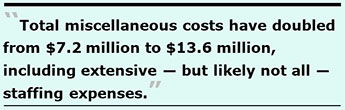
Back in July 2023, Table 4 below had shown at the time just $7.2 million across 16 miscellaneous itemized projects. Of those 16 items, one has now been moved into a new table (Table 5), and another five items have been moved to another new table (Table 6). In their place, six additional items have been added to Table 4 (or on-line). Total miscellaneous costs have doubled from $7.2 million to $13.6 million, including extensive — but likely not all — staffing expenses.
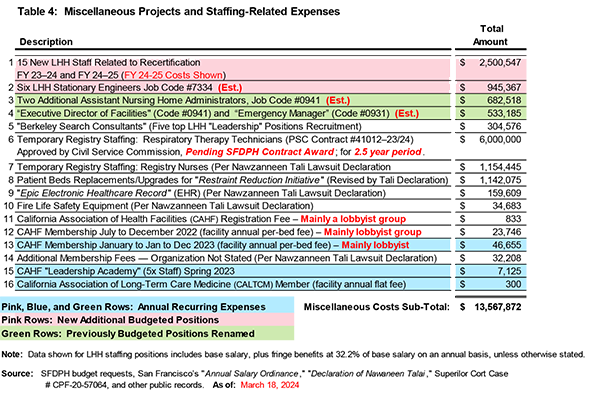
A few items in Table 4 deserve attention:
 The upshot is the $1.15 million in expenses for temporary nursing staff registry contracts listed in Row 7 of Table 4 — which was inadvertently revealed on page 7 in a declaration filed by LHH’s Chief Quality Officer, Nawzaneen Tali on March 18, 2024 in a lawsuit against LHH — is totally under-reported, when not pure fiction. After all, LHH has at least 820 nursing staff (including RN’s, LVN’s, PCA’s, and CNA’s, along with various nurse managers and nursing supervisors). It’s not possible to have pulled those 820 Nursing staff from performing their direct patient care duties to attend multiple training and re-training sessions over an entire two-year period and spent only a mere $1.15 million hiring the temporary employees to fill in while regular employees were attending training classes.
The upshot is the $1.15 million in expenses for temporary nursing staff registry contracts listed in Row 7 of Table 4 — which was inadvertently revealed on page 7 in a declaration filed by LHH’s Chief Quality Officer, Nawzaneen Tali on March 18, 2024 in a lawsuit against LHH — is totally under-reported, when not pure fiction. After all, LHH has at least 820 nursing staff (including RN’s, LVN’s, PCA’s, and CNA’s, along with various nurse managers and nursing supervisors). It’s not possible to have pulled those 820 Nursing staff from performing their direct patient care duties to attend multiple training and re-training sessions over an entire two-year period and spent only a mere $1.15 million hiring the temporary employees to fill in while regular employees were attending training classes. Behavioral Health Response Team
Also by the middle of September, it became clear the four major categories of spending I had started out with in July 2023 needed to expand to add the Behavioral Health category.
Table 5 below (or on-line) sshows at least 51.6 full-time equivalent (FTE) staff had to be added to help manage the behavioral health cohort of patients inappropriately shunted into Laguna Honda who have, or had, substance abuse and mental health diagnoses that other Laguna Honda Hospital staff were unable to care for safely, and provide those behavioral health patients with the healthcare services they deserve to have. Two-thirds of the 52 additional staff were private security staff, not City employees.
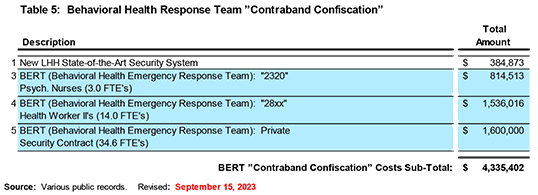
It’s unclear to what extent the rows highlighted in blue shading were one-time expenses, or whether they represent on-going annual expenses into future years.
Importantly, a decision about whether to split LHH into two types of facilities — a long-term care skilled nursing facility that LHH has served as for 150 years, vs. a separate “behavioral health facility” — by placing the skilled nursing patients in one of LHH’s patient towers, and placing the “behavioral health” patients in the other patient tower to physically separate them somewhat to prevent adverse interactions, has not yet been finalized. Comingling the two patient populations in the same facility is referred to as “cohorting.”
 It’s not yet known whether once LHH gains its recertification whether its space for “behavioral health” patients will be expanded, because a workgroup assigned to evaluate that possibility hasn’t presented its overdue report to San Francisco’s Health Commission.
It’s not yet known whether once LHH gains its recertification whether its space for “behavioral health” patients will be expanded, because a workgroup assigned to evaluate that possibility hasn’t presented its overdue report to San Francisco’s Health Commission.
Although some sort of potentially interdisciplinary “study group” at SFDPH has been analyzing this issue as a pending policy decision for over a year, the study group’s report that was supposed to have been presented to San Francisco’s Health Commission has not been made yet. LHH’s former “interim-CEO,” Roland Pickens, has gone completely radio silent on this issue and hasn’t kept the Health Commission informed about the status of that pending “analysis” for months. And of course, the Health Commission has been too lazy to have even asked proactively about why that report has been delayed.
It’s not yet known if that “cohorting” decision will be made after LHH gains its CMS recertification and re-opens for patient admissions that have been halted for two years.
To the extent any plan to reconfigure LHH to handle patients with primary mental health diagnoses in a “mental health rehabilitation facility” crammed into one of LHH’s two patient towers comes to fruition, costs above the $4.3 million shown in Table 5 above will soon occur, likely substantially.
So-Called “Emergency Repairs” Costs
Also by the middle of last September, it became clear the four major categories of spending I had started out with in July 2023 needed to expand to a sixth main category for so-called “emergency repairs” to LHH’s facilities. It’s not clear that all of the projects listed in Table 6 are actually required by CMS in order to grant recertification of LHH to participate in the Medicare and Medicaid provider program.
In actuality, these projects are not so much “emergency repairs” as they are long-neglected, long deferred-maintenance repairs, including construction problems from the rebuild of the new LHH facilities that had opened in June 2010.
The “emergency repairs” consist of at least 16 separate projects shown in Table 6 (or on-line).
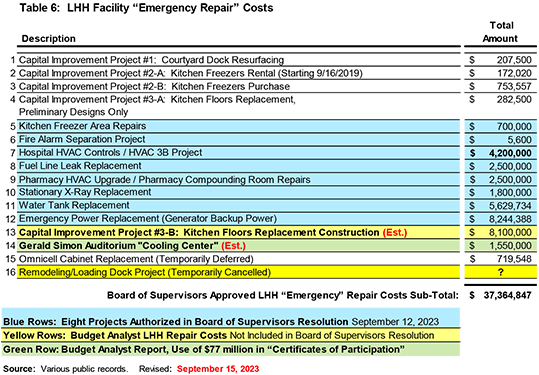
 Notably, in early September 2023 — after returning from its month-long summer recess last August to figuratively vacation in Cancun with U.S. Senator Ted Cruz — the Board of Supervisors quibbled over, and altered, the order of priority of eight of the 16 repair projects. That’s because the Board’s Budget and Legislative Analyst (BLA) — the Harvey Rose Consultancy corporation — had originally prepared a BLA report recommending eight priority LHH repair projects. But for some reason SFDPH and/or Laguna Honda decided to quibble with the Board of Supervisors, and several of the projects the BLA had recommended were swapped out with a final list of eight LHH projects the Board of Supervisors ended up passing as an “Emergency Declaration” in Resolution #422-23.
Notably, in early September 2023 — after returning from its month-long summer recess last August to figuratively vacation in Cancun with U.S. Senator Ted Cruz — the Board of Supervisors quibbled over, and altered, the order of priority of eight of the 16 repair projects. That’s because the Board’s Budget and Legislative Analyst (BLA) — the Harvey Rose Consultancy corporation — had originally prepared a BLA report recommending eight priority LHH repair projects. But for some reason SFDPH and/or Laguna Honda decided to quibble with the Board of Supervisors, and several of the projects the BLA had recommended were swapped out with a final list of eight LHH projects the Board of Supervisors ended up passing as an “Emergency Declaration” in Resolution #422-23.
See public testimony submitted to the Board of Supervisors that compared the names of the eight projects the BLA had analyzed and had recommended, vs. the eight projects the Board of Supervisors eventually approved — with the Board of Supervisors’ clear proviso that the repair costs were not to exceed $28.4 million!
Three of the projects the BLA had recommended — a “Hospital HVAC Controls” project, “Pharmacy HVAC Upgrade” project, and a “Kitchen Floor Replacement” project, each with stated estimated costs — were replaced by three other projects the Board of Supervisors added: a “Fire Alarm Separation” project, “HVAC 3B” project, and a “Pharmacy Room Compounding Room Repairs” project, all having estimated costs of zero dollars! How could the Board of Supervisors have allocated funding to three explicitly-named projects without knowing what they would likely potentially cost? (That’s a question to ask Supervisors Peskin, Chan, and Melgar.)
![]() Indeed, the kitchen floor replacement project that the BLA had recommended for funding — but which the Board of Supervisors in their infinite wisdom completely eliminated from their final Resolution — should have been fixed over a decade ago!
Indeed, the kitchen floor replacement project that the BLA had recommended for funding — but which the Board of Supervisors in their infinite wisdom completely eliminated from their final Resolution — should have been fixed over a decade ago!
That’s because the pathetically-low $15.3 million the City recovered as a settlement of the Anshen + Allen and Stantec LHH rebuild architectural partners lawsuit was deposited into the City’s General fund, but notused to immediately repair LHH’s kitchen floor, even though the defective kitchen floor had been a prominent complaint in the lawsuit. Alternatively, since Stantec was not released from any further lawsuits and liability from “latent defects,” LHH’s defective kitchen floor should have been repaired long before now using a “latent defect” funding source, and not need taxpayers footing the bill using more scarce Capital Improvement Funds, or the $28.4 million in emergency repair funds the Board of Supervisors passed.
The kitchen floor replacement project had been identified as a critical project shortly after the LHH replacement hospital opened in 2010 and severe mold soon appeared in LHH’s brand-new kitchen, as a result of poor architectural design of the kitchen floor using glass in the floor tiles. It’s disgraceful it has taken over a dozen years to begin replacement of LHH’s kitchen floor after it was identified as a problem as early as 2011. All along, LHH had declined to provide an estimated date on when the floor replacement would begin or might be completed in order to ensure LHH successfully passes CMS and CDPH recertification inspections.
 When the Board of Supervisors claimed the spending would involve a “not-to-exceed” amount of $28.4 million, it was obviously a lie in September 2023, and it’s a proven lie now. That’s because the March 18 Tali declaration also reported on page 7 that LHH has already spent $3.3 million in capital repair costs and is planning to spend another $26.7 million on repairs “necessary for recertification.” That totals $29.97 million, not the $28.4 million not-to-exceed amount the Board of Supervisors tried to palm off via a lie in September 2023.
When the Board of Supervisors claimed the spending would involve a “not-to-exceed” amount of $28.4 million, it was obviously a lie in September 2023, and it’s a proven lie now. That’s because the March 18 Tali declaration also reported on page 7 that LHH has already spent $3.3 million in capital repair costs and is planning to spend another $26.7 million on repairs “necessary for recertification.” That totals $29.97 million, not the $28.4 million not-to-exceed amount the Board of Supervisors tried to palm off via a lie in September 2023.
Table 6 above shows those facility repair costs will more probably cost $39 million, and certainly not the $28.4 million the Board of Supervisors (including Supervisor Connie Chan, Chair of the Board’s Budget Committee; Board President Aaron Peskin; and District 7 Supervisor Myrna Melgar) would like you to believe — pulling the wool over your eyes.
![]() A Costly Anniversary Gift
A Costly Anniversary Gift
The entire $$125 million $177.5 million to $152.3 million $204.8 million in expenses to rescue Laguna Honda Hospital outlined in this article might have been avoided entirely, had San Francisco’s Health Commission adequately performed its role as LHH’s “governing body.”
And given several caveats discussed throughout this article — including significant unknown millions in costs for registry staffing to replace nurses while they were undergoing training and re-training, massive costs in City Attorney time and expenses during the past two-½ to three years, and outstanding lawsuit settlements remaining against the City — the more probable costs to rescue Laguna Honda probably approaches somewhere between $175 million $204.8 million and $200 million $250 million, given the yet unknown expenses still accumulating.
These millions in expenses represent a sad anniversary gift, now that we’ve reached the second anniversary of LHH’s decertification on April 14, 2022.
Sadly, neither LHH’s inept senior managers nor San Francisco’s “governing body” Health Commission who directly caused or obviously contributed to the waste of millions of dollars in City resources have been adequately held responsible or were terminated.
More sadly, as of this writing, LHH has not been recertified, patient admissions have not restarted so patients needing skilled nursing care are still being displaced into out-of-county facilities, and San Franciscans still haven’t been told whether LHH will also lose 120 of its 769 skilled nursing beds demanded by CMS as further punishment — which would not have even been on the table had LHH never been decertified in April 2022.
 All of which was set in motion during the disastrous 2019 patient sexual abuse scandal under former LHH CEO Mivic Hirose’s culture of silence watch during her reign of mismanagement, and her self-admitted failure to enact a culture of patient safety.
All of which was set in motion during the disastrous 2019 patient sexual abuse scandal under former LHH CEO Mivic Hirose’s culture of silence watch during her reign of mismanagement, and her self-admitted failure to enact a culture of patient safety.
Monette-Shaw is a columnist for San Francisco’s Westside Observer newspaper, and a retired City employee. He received a James Madison Freedom of Information Award in the “Advocacy” category from the Society of Professional Journalists–Northern California Chapter in 2012. He’s a member of the California First Amendment Coalition (FAC) and the ACLU. Contact him at monette-shaw@westsideobserver.com.