 Printer-friendly PDF file
Printer-friendly PDF file
Westside Observer
Newspaper
December 2019 – January 2020 at www.WestsideObserver.com
Patient Safety Endangered by Cultural Wall of Silence
LHH Leadership Fingered in Patient Abuse Scandal
by Patrick Monette-Shaw
Here we are six months after first learning from Mayor London Breed on June 28, 2019 about the outrageous abuse of 23 patients at Laguna Honda Hospital (LHH) dating back to 2016. We’re no closer to getting answers about key questions because the scandal remains shrouded in secrecy and remains an on-going State investigation.
On October 23, LHH’s leadership was finally fingered during a Board of Supervisors Government Audit and Oversight (GAO) hearing as having been a primary contributor to the patient abuse, and failure to report the abuse.
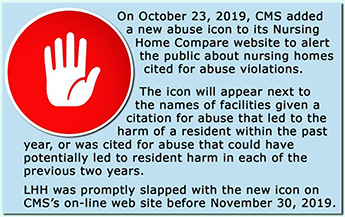
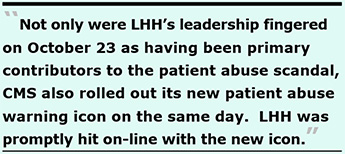 Ironically, also on October 23, the Centers for Medicare and Medicaid Services (CMS) rolled out its new warning icon on its Nursing Home Compare website to alert consumers about long-term care facilities at which patient abuse had been uncovered. LHH was promptly hit with the new icon by CMS somewhere between October 23 and November 30, 2019. Thanks, “leaders”!
Ironically, also on October 23, the Centers for Medicare and Medicaid Services (CMS) rolled out its new warning icon on its Nursing Home Compare website to alert consumers about long-term care facilities at which patient abuse had been uncovered. LHH was promptly hit with the new icon by CMS somewhere between October 23 and November 30, 2019. Thanks, “leaders”!
CMS initially assigned the abuse icon to 56 (4.7%) of California’s 1,193 CMS-certified nuring facilities. That’s not good company for LHH — or LHH’s patients — to be in.
A culture of patient safety is particularly vulnerable to fatality if it collides with a culture of silence speeding out of control, careening throughout a hospital for over a decade-and-a-half. The heart of the problem involves polar opposite cultures.
 Toss in the nonsensical word-salad pabulum from Health Commissioner Dr. Ed Chow about a totally unrelated problem involving cultural humility, and you know there’s a real problem of culture and a likelihood the conspiracy of silence will prevail. Some observers believe the problems at LHH definitely involved a conspiracy of silence across multiple departments, including its Nursing Department and its Medical Services Department.
Toss in the nonsensical word-salad pabulum from Health Commissioner Dr. Ed Chow about a totally unrelated problem involving cultural humility, and you know there’s a real problem of culture and a likelihood the conspiracy of silence will prevail. Some observers believe the problems at LHH definitely involved a conspiracy of silence across multiple departments, including its Nursing Department and its Medical Services Department.
On November 19, Supervisor Norman Yee was reported to have asked, “What the heck are we waiting for?” in an unrelated issue involving delays implementing safety measures to prevent injuries and deaths of pedestrians and bicyclists involved in traffic crashes.
When it comes to investigations into patient abuse and patient safety at Laguna Honda Hospital (LHH) announced over six months ago, I have my own questions for Yee: “What the heck is taking so long to implement a culture of patient safety at LHH? What were you waiting for? The red-hand CMS warning icon?”
 Patient Abuse Scandal Erupts
Patient Abuse Scandal Erupts
San Franciscans first learned of the staff abuse of LHH patients in a San Francisco Examiner article on June 28 reporting a press conference Mayor London Breed held with Supervisor Norman Yee and the new Director of Public Health (DPH), Dr. Grant Colfax to announce the scandal. During the press conference, Dr. Colfax claimed he was concerned about the culture of silence that allowed the patient abuse to have gone unreported and continued for so long.
The Examiner article reported LHH’s CEO, Mivic Hirose, had stepped down and that LHH’s Director of Quality Management (DQM) had also been “removed.” DPH refused to name the DQM, claiming it was a personnel matter. That’s preposterous.
First, Googling “Who is the director of quality management at LHH” returns information and Health Commission public records showing that Regina Gomez was LHH’s DQM. Googling “Regina Gomez San Francisco” returns a link that takes you to her LinkedIn profile that lists she had been LHH’s DQM. Her full LinkedIn profile appears to have recently been taken down and only a snippet of it remains on-line. Meeting minutes of the Health Commission’s Joint Conference Committee with LHH’s leadership team show Gomez frequently presented Quality Management reports during LHH-JCC meetings.
Second, public employees typically do not have “employee privacy rights.” Facilities must disclose basic information about city employee salaries and work locations, although their disciplinary records may not be subject to disclosure (now, only police officer disciplinary records must be disclosed, at least in part).
Initial reporting claimed just 23 patients had allegedly been abused over the past three years dating back to 2016. Breed indicated the abuse was uncovered in February 2019 only because of a DPH investigation into an unrelated sexual harassment complaint filed by an LHH employee and stumbled across the potential evidence of patient abuse. The City Attorney’s Office assisted in DPH’s investigation. The initial article indicated that both the California Department of Public Health (CDPH) and the SFPD Special Victims Unit were also conducting investigations.
Remarkably, Dr. Colfax stated during the press conference “We immediately started an internal investigation and found evidence to substantiate our initial suspicion.” It was a stupid thing for Colfax to have said, because we later learned that a doctor at an external acute care hospital had e-mailed LHH’s Medical Director, Dr. Michael Mcshane, as far back as February 26, 2018 about an LHH patient who had stopped breathing and was transported to an acute care hospital on February 13, 2018 with life-threatening problems related to an overdose of opioids she had not been prescribed.
 Mcshane replied to the UCSF doctor that an internal investigation into the case was underway. Nine months later, the same patient was again transferred on October 26, 2018 to an acute care hospital because of mental status changes as a result of other medications which had also not been prescribed. A second LHH patient who had also stopped breathing and had respiratory arrest was transported to an acute care hospital on January 8, 2018. A different acute hospital doctor had been told LHH’s staff was investigating the second case. So, Colfax should have known that rather than starting an investigation in February 2019, LHH had purportedly been investigating for over a year. Colfax should also have known that a third patient wrongly administered opioids he had not been prescribed died on September 2, 2018.
Mcshane replied to the UCSF doctor that an internal investigation into the case was underway. Nine months later, the same patient was again transferred on October 26, 2018 to an acute care hospital because of mental status changes as a result of other medications which had also not been prescribed. A second LHH patient who had also stopped breathing and had respiratory arrest was transported to an acute care hospital on January 8, 2018. A different acute hospital doctor had been told LHH’s staff was investigating the second case. So, Colfax should have known that rather than starting an investigation in February 2019, LHH had purportedly been investigating for over a year. Colfax should also have known that a third patient wrongly administered opioids he had not been prescribed died on September 2, 2018.
An on-line comment posted to the Examiner’s June 28 article was submitted by Dr. Maria Rivero, a former LHH doctor. Rivero wrote:
“Anyone who spoke out about patient concerns under Hirose lost their jobs; that was well known to the entire DPH. Disgraced administrators should lose their Fat City Pensions. That is the best deterrent to this type of problem.”
The issue of pensions resurfaced in late October, discussed further, below.
Additional Media Coverage
Following the Examiner’s initial June 28 article, a number of consecutive media reports surfaced:
- A second Examiner article was published on September 6, describing the sordid details that had emerged about the patient abuse scandal in a 61-page report from CDPH known as a facility survey conducted and completed on July 12, 2019. The article noted abuse remains under investigation by San Francisco’s Police Department. CPDH’s 61-page report noted an unidentified LHH nurse manager told CDPH investigators that the abuse incidents had came to light only because of an LHH staff member’s February 2019 complaint reporting on-the-job sexual harassment, ignoring external acute care hospital doctors had been told back in February 2018 that LHH was conducting an investigation into patients transferred to area hospitals with life-threatening symptoms from medication overdoses.
CDPH’s report noted that LHH had “failed to report the patient abuse in a timely manner to CDPH.” Since LHH’s Quality Management Department is responsible for reporting abuse to CDPH, you have to wonder whether Gomez was removed as DQM because of the failure to report abuse to CDPH within two hours of incidents, as required.
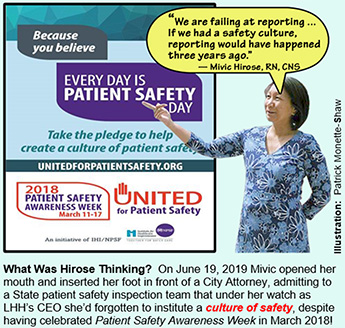
CDPH’s survey report noted Hirose had stupidly told the state patient safety inspectors on June 19, 2019 during a survey interview attended by DQM Regina Gomez, LHH’s Director of Nursing Madonna Valencia, and a Deputy City Attorney:
“… I wish all of these [incidents] were reported in 2016 when some of the resident’s pictures were taken ... we are failing at reporting … If we had a safety culture, reporting would have happened three years ago …”
 Mivic should have known after having been either LHH’s Co-Director or sole Director of Nursing for 10 years, and after having been LHH’s CEO for an additional decade, that submitting patient abuse reports to CDPH within two hours was not optional, but a mandatory, ministerial requirement to promote a culture of safety. What was she thinking making such a ridiculous admission? There should have been a culture of reporting, along with a culture of patient safety. Furthermore, LHH’s annual report for Fiscal Year 2017–2018 contained an illustration shown at the top of this article that LHH had celebrated Patient Safety Awareness Week April 11 through April 17, 2018. How could Hirose have missed that celebration?
Mivic should have known after having been either LHH’s Co-Director or sole Director of Nursing for 10 years, and after having been LHH’s CEO for an additional decade, that submitting patient abuse reports to CDPH within two hours was not optional, but a mandatory, ministerial requirement to promote a culture of safety. What was she thinking making such a ridiculous admission? There should have been a culture of reporting, along with a culture of patient safety. Furthermore, LHH’s annual report for Fiscal Year 2017–2018 contained an illustration shown at the top of this article that LHH had celebrated Patient Safety Awareness Week April 11 through April 17, 2018. How could Hirose have missed that celebration?
During that same June 19 interview with CDPH investigators, DQM Gomez stupidly stated “… It has been mind blowing these incidents happened … we did not see any signs …” How could Gomez not have known about the five LHH patients transferred to acute care hospitals with life-threatening complications from opioids wrongly administered? Had Mcshane not notified Gomez about the “signs” he had received from external hospital MD’s?
Also, during that same June 19 interview with CDPH investigators, LHH’s Chief Nursing Officer, Madonna Valencia, stated:
“… Yes, some of the incidents are possibly a crime against residents; we reported them to law enforcement when we became aware [of them] …”
 Valencia’s name was also uncovered from a simple Google search.
Valencia’s name was also uncovered from a simple Google search.
It’s not clear on what date LHH first began reporting patient abuse problems to law enforcement agencies, or for the matter, resumed reporting them to CDPH as it was required to do.
Worse, an earlier CDPH survey report dated October 15, 2018 about different LHH patient incidents reported that Valencia may have provided untruthful information to CDPH — and perhaps to a patient’s family — that LHH had never had a hospice unit:
“In an interview with the Director of Nursing (DON) on [DATE 2018] at 10 AM, she stated the facility does not have contracts with hospices. The DON stated there has never been a hospice unit in either the old [LHH finger-wing] building or the new [replacement hospital opened in 2010] where all the residents now reside. The DON said they have a contract with a hospice but only to provide volunteers, not the other hospice services … the DON stated she would be open to exploring hospice services.”
Valencia was first hired at LHH on August 22, 1999 about six months after I had been hired by Dr. Rivero. On November 10, 2001 Madonna was promoted to being a Nurse Manager and eventually became Nurse Manager on the Rehabilitation Unit on Ward K-4 where I supported her in the Medical Rehab Services Department. I, along with many clinicians in the Rehab Services Department, believed she was a competent Nurse Manager/ who came informed and well prepared to discuss individual patients undergoing physical medicine rehabilitation during weekly patient case conference meetings.
Valencia had to have known as early as 1999 when she was first hired — as I did — of Dr. Derek Kerr’s award-winning Hospice Unit on C-2. She can not possibly have not known LHH had that hospice unit.
Maddeningly, the September 6 article revealed Colfax wasn’t the only senior leader of DPH making stupid statements. The Examiner article reported on the September 3, 2019 Health Commission meeting during which an “LHH Turn-Around Reform Plan” was presented. That’s when Health Commissioner Dr. Chow stupidly blurted out his nonsense about the need for a greater emphasis on cultural humility during the employee recruitment process. Chow asserted the lack of cultural humility may have been at the core of the patient abuse at LHH. Cultural humility refers to:
“Cultural humility, a process of reflection and lifelong inquiry, involves self-awareness of personal and cultural biases as well as awareness and sensitivity to significant cultural issues of others.”
It should not take self-humility or cultural humility for nursing staff or medical staff to understand that administering opioids to patients who hadn’t been prescribed them, and other forms of patient abuse, have nothing to do with cultural biases or a lack of exposure to people of other cultural backgrounds. It should be apparent that every culture has a significant issue of not killing patients, however inadvertently.
If a nurse or certified nursing assistant isn’t taught that opioid overdoses can lead to killing a patient and that they can lose their licenses to be nurses, then they have no business being nurses in the first place, with or without a dose of cultural humility. You don’t need to have cultural humility in order to provide a culture of patient safety! That’s just word-salad nonsense from the so-called esteemed Dr. Chow.
- A third Examiner article was published five days later on September 11, indicating Hirose was still employed by the City as a clinical nurse specialist in the Information Technology Unit after she had resigned as LHH’s CEO.
In response to a records request I placed on September 8, DPH confirmed on the same day as the Examiner’s September 11 article, that Hirose had been re-assigned:
“… to help implement the “Epic” Electronic Health Record (EHR). DPH claimed ‘the Informatics Clinical Nurse Specialist works in the continuing development of the EHR as an effective clinical tool aligning the platform with evidence-based best-practice and optimizing workflows. She is part of the Clinical Informatics team responsible for designing, configuring, testing, implementing and training clinical and financial aspects of the EHR’.”
 Problem is, a “Contemporary Letter” way back on April 21, 2009 shows Hirose’s Clinical Nurse Specialty is not in “informatics” or information technology. Her clinical experience and specialty was in Medical-Surgical/Trauma. It’s not known if Hirose has ever received training in, or credentials as, an Informatics Clinical Nurse Specialist. Her specialty and job experience had been as a surgical staff nurse, and as a Surgical/Trauma Clinical Nurse Specialist.
Problem is, a “Contemporary Letter” way back on April 21, 2009 shows Hirose’s Clinical Nurse Specialty is not in “informatics” or information technology. Her clinical experience and specialty was in Medical-Surgical/Trauma. It’s not known if Hirose has ever received training in, or credentials as, an Informatics Clinical Nurse Specialist. Her specialty and job experience had been as a surgical staff nurse, and as a Surgical/Trauma Clinical Nurse Specialist.
The Examiner’s September 11 article reported Dr. Kerr said he doesn’t believe Hirose was “entirely responsible” for the patient abuse. Kerr may be right. But DPH administrators, however, later determined before October 23 that LHH’s leadership were primary contributors to the patient abuse. They may not have been entirely responsible, but they certainly contributed to the abuse scandal. Kerr noted:
“At Laguna Honda, there are a number of cultural factors that [work against] speaking out, one of which has been the adversarial attitude towards whistleblowers and critics. That intimidates everybody else.”
The September 11 article also quoted me:
“[Hirose], in my opinion, should never have been appointed as [LHH’s] chief executive officer. She never had experience running an entire hospital. I don’t think she was qualified to ever be appointed CEO.”
 “Class AA” Violations
“Class AA” Violations
Long-term care skilled nursing facilities risk losing their licenses if they receive a second, subsequent “Class AA” citation that has been sustained within a 24-month period following a citation review conference and following receipt of a first “Class AA” citation.
“Class AA” citations and fines result from abuse or neglect violations that CDPH “determined to have been a direct proximate cause of death of a patient or resident of a long term care facility.”
Some observers wonder whether the patient abuse went unreported to CDPH because LHH was then under a two-year period during which it could lose its license completely if it received a second “Class AA” citation from CDPH.
 LHH had received a “Class AA” citation and a $100,000 fine on December 23, 2016. As early as November 2, 2017 — within the first year — one of the five patients who had been drugged tested positive for Methadone he hadn’t been prescribed. He was drugged eight additional times with different opioids through August 2018. He died on September 2, 2018 while the two-year period for the 2016 “Class AA” citation was still in effect. It’s probable LHH may end up receiving another “Class AA” citation for his death thanks, in part, to Hirose’s “leadership.”
LHH had received a “Class AA” citation and a $100,000 fine on December 23, 2016. As early as November 2, 2017 — within the first year — one of the five patients who had been drugged tested positive for Methadone he hadn’t been prescribed. He was drugged eight additional times with different opioids through August 2018. He died on September 2, 2018 while the two-year period for the 2016 “Class AA” citation was still in effect. It’s probable LHH may end up receiving another “Class AA” citation for his death thanks, in part, to Hirose’s “leadership.”
It should be noted City Attorney Dennis Herrera filed a Superior Court lawsuit against CDPH on April 13, 2017 seeking to have the December 2016 “Class AA” citation dismissed and the $100,000 fine eliminated, arguing CDPH was “untimely” by having issued the citation five months after coimpleting its 2016 facility survey, rather than issuing the citation within 30 days. That’s just more hogwash! It took until January 22, 2019 before a Court filing announced a proposed settlement had been reached to reduce the citation to a “Class A” citation (one “A,” instead of two) but kept the $100,000 fine. The proposed settlement was contingent on approval by the Health Commission, Board of Supervisors, and the Mayor.
 After the Health Commission approved the settlement, it then took the Board of Supervisors until November 5, 2019 to pass an Ordinance on second reading agreeing to pay the $100,000 fine, and ostensibly approve the settlement. It’s not known on what date Mayor Breed may have approved the settlement.
After the Health Commission approved the settlement, it then took the Board of Supervisors until November 5, 2019 to pass an Ordinance on second reading agreeing to pay the $100,000 fine, and ostensibly approve the settlement. It’s not known on what date Mayor Breed may have approved the settlement.
As late as December 3, 2019 the City Attorney’s Office claims it still cannot disclose the dollar amount of city attorney time and expenses incurred in the lawsuit against CDPH during the two-and-a-half years since Herrera filed it in April 2017, because the matter isn’t fully closed:
“Unfortunately, we cannot provide the requested information at this time because the matter is not yet closed. Having Board of Supervisor authorization to settle a case does not necessarily conclude everything to the point that a matter can be closed. You may check back toward the beginning of the new year to see if the closing process is finished by that point; however, we cannot make any predictions or guarantees. Until the matter, is closed, the requested information is exempt as attorney work product.”
 Because the lawsuit isn’t “officially” fully closed, it’s not clear on what date, if any, CDPH’s two-year period for “Class AA” violations may have stopped, or whether CDPH’s two-year clock had remained ticking at the time Patient 11 died in September 2018. Thanks, Mivic!
Because the lawsuit isn’t “officially” fully closed, it’s not clear on what date, if any, CDPH’s two-year period for “Class AA” violations may have stopped, or whether CDPH’s two-year clock had remained ticking at the time Patient 11 died in September 2018. Thanks, Mivic!
Sadly, it’s not known how soon CDPH will conclude its investigation of LHH and whether it will issue, yet again, another “Class AA” ruling and accompanying State fine. The California Advocates for Nursing Home Reform (CANHR) reported on October 24 that CDPH has an enormous backlog of open complaints and facility reports of abuse — over 17,000 cases — some of which were reported years ago.
In the movie Queen of Outer Space (1958), Zsa Zsa Gabor wryly opined, “soufflé is for people without teeth.” When it comes to rapid and timely investigations of abuse in California nursing homes, CDPH appears to be eating soufflé, having no teeth!
 Fines and Penalties Against LHH
Fines and Penalties Against LHH
On September 3, the federal Centers for Medicare and Medicaid Services (CMS) imposed a $1 million fine against LHH for the 156 days between February 6 and July 11, 2019 during which patient’s health and safety were in immediate jeopardy. Since 2007, LHH has been fined at least $1.5 million, but has only had to pay $1 million because it received a handful of 35% discounts by waiving its rights and not contesting the determinations and fines. The fines are expected to soar significantly higher.
Table 1: Fines and Penalties LHH Has Paid to CMS and CDPH
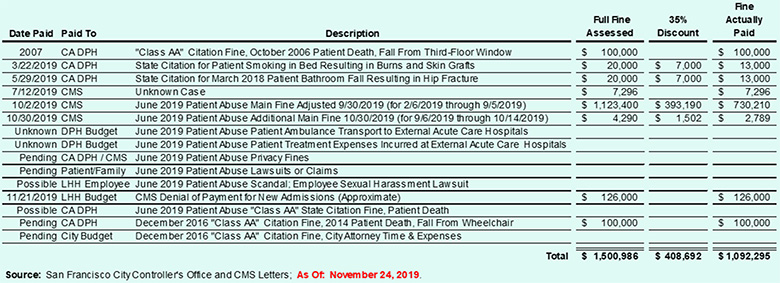
It may take several years before any of the blank lines in Table 1 become known.
 What this suggests is that although there were fines imposed for patients wrongly administered opioid-level meds they had not been prescribed, no fines may have been imposed for other patients who were prescribed meds that they may never have received. Again, not to put too fine a point on this, harm was caused to both patients drugged without orders, and more harm was caused to patients who may not have received their pain control meds. Didn’t Hirose — or CDPH, SFDPH, the Health Commission, or the Board of Supervisors — notice this glaring problem?
What this suggests is that although there were fines imposed for patients wrongly administered opioid-level meds they had not been prescribed, no fines may have been imposed for other patients who were prescribed meds that they may never have received. Again, not to put too fine a point on this, harm was caused to both patients drugged without orders, and more harm was caused to patients who may not have received their pain control meds. Didn’t Hirose — or CDPH, SFDPH, the Health Commission, or the Board of Supervisors — notice this glaring problem?
In addition to the $1 million in fines actually paid out, lawsuits filed by at least two LHH employees since 2010 have resulted in nearly $1.5 million in additional costs to LHH and DPH. Between the lawsuit filed by Cheryl Austin and the wrongful termination lawsuit filed by Dr. Derek Kerr, LHH had to pay out a little over $1 million in settlements to the two employees, plus another $468,585 in City Attorney time and expenses trying to stop their lawsuits, for a total of $1,487,037. LHH’s former CEO, John Kanaley, was responsible for Austin’s racial discrimination and retaliation lawsuit, and Hirose was principally responsible for Kerr’s wrongful termination and whistleblowing lawsuit.
Between the $1.5 million in full fines assessed, and the $1.5 million in employee lawsuit costs, we’re up to at least $3 million in “leadership” problems at LHH. That $3 million is probably far higher. What took so long to sack Hirose? Didn’t the Health Commission, or the Board of Supervisors, or the Director of Public Health notice the increasing costs under her problematic “leadership”?
The Patients Abused
Although Breed initially claimed 23 patients were involved in the abuse, DPH eventually admitted 130 patients had been affected in different ways in violation of state and federal law. LHH admitted on October 25 that 30 patients had been abused by “chemical restraint” (drugging), sexual-related abuse, and physical or verbal abuse. Another 25 patients had been photographed or were visible in photographs, which amounted to privacy violations. Another 75 patients had their names, but not their photos, disclosed in recordings and text messages, also privacy violations.
 On October 23, the Board of Supervisors were advised (below) that additional fines against the hospital are still expected because privacy fines take more time, and are typically steep.
On October 23, the Board of Supervisors were advised (below) that additional fines against the hospital are still expected because privacy fines take more time, and are typically steep.
I want to focus here on the five patients who were hospitalized with life-threatening conditions following administration of non-prescribed medications, and were not protected and kept free from “Chemical Restraints,” because that was particularly egregious.
Repeating the link, the CDPH survey of LHH revealed that five patients who developed life-threatening conditions were transferred to acute care hospitals for over-sedation, respiratory depression, and/or altered mental status after receiving medications they had not been prescribed.
The survey reported that a Licensed Vocational Nurse (LVN) and a Certified Nursing Assistant (CNA) intentionally administered non-prescribed medications for staff convenience.
The five residents were:
- Resident 6
On February 13, 2018 paramedics bagged Resident 6 in an ambulance en route from LHH to an acute care hospital, and administered a 1 mg dose of Naloxone (Narcan®) to reverse the effects of opioid overdose. (Bagged refers to forcing oxygen into a patient’s lungs after they stop breathing.) Resident 6’s urine toxicology (u-tox) screen on admission to the acute care hospital tested positive for Methadone, Morphine, Tramadol, Gabapentin, and Quetiapine, which all cause sedation. The first three drugs can also cause respiratory depression, which is potentially life threatening and a cause of substantial mortality.
 On February 26, 2018 an MD at the acute care hospital concerned about Resident 6’s presenting circumstances e-mailed LHH Medical Director, Dr. Michael Mcshane, reporting the u-tox results. According to the state survey report, Mcshane reportedly replied indicating that an internal investigation was underway at LHH. The acute care hospital MD also e-mailed the final comprehensive toxicology report to Mcshane on March 5, 2018.
On February 26, 2018 an MD at the acute care hospital concerned about Resident 6’s presenting circumstances e-mailed LHH Medical Director, Dr. Michael Mcshane, reporting the u-tox results. According to the state survey report, Mcshane reportedly replied indicating that an internal investigation was underway at LHH. The acute care hospital MD also e-mailed the final comprehensive toxicology report to Mcshane on March 5, 2018.
Nine months later, Resident 6 was transferred again from LHH to an acute care hospital on October 26, 2018 for facial droop and mental status changes. His October 30, 2018 u-tox screen tested positive for benzodiazepines, which he had also not been prescribed.
Benzodiazepines are prescription sedatives or tranquilizers classified as Schedule IV in the Controlled Substances Act. Benzo’s can cause acute cognitive impairment, and are highly addictive. Benzo overdose can be fatal if they are mixed with opioids.
- Resident 24
On August 8, 2018 Resident 24 was transferred to an acute care hospital suffering respiratory failure. Both Methadone and Tramadol, which had not been prescribed, were detected by her u-tox screen.
- Resident 25
On December 25, 2018 Resident 25 was transferred to an acute care hospital with “over sedation” and altered mental status, and placed on breathing support in an ICU. Her toxicology lab reports tested positive for Mirtazapine (an antidepressant) and Gabapentin (an anti-seizure medication); both medications cause sedation. She had not been prescribed either medication. Resident 25’s u-tox screen two weeks later again tested positive for Gabapentin on January 7, 2019.
- The Death of Resident 11
 Resident 11 was viewed by the LVN and CNA as a “difficult” resident and may have been administered non-prescribed meds “to put him to sleep” to render him less difficult “for their convenience.” The State survey did not report a specific date on which Resident 11 was transferred to an acute care hospital. Resident 11 did have a physician’s order for weekly urine toxicology screens. Resident 11 first tested positive for Methadone on November 2, 2017 and tested positive eight more times between January 17 and August 6, 2018 for Morphine, Methadone, and Oxycodone. One of the tox screens identified both Oxycodone and Morphine; another tox screen identified both Morphine and Methadone.
Resident 11 was viewed by the LVN and CNA as a “difficult” resident and may have been administered non-prescribed meds “to put him to sleep” to render him less difficult “for their convenience.” The State survey did not report a specific date on which Resident 11 was transferred to an acute care hospital. Resident 11 did have a physician’s order for weekly urine toxicology screens. Resident 11 first tested positive for Methadone on November 2, 2017 and tested positive eight more times between January 17 and August 6, 2018 for Morphine, Methadone, and Oxycodone. One of the tox screens identified both Oxycodone and Morphine; another tox screen identified both Morphine and Methadone.
Resident 11 expired — died — on September 2, 2018 almost a month after the August 6 tox screen. It isn’t known if a post-mortem tox screen was performed, or tested positive for any of the three meds, since they are undetectable in urine three to four days after administration.
The LVN and CNA appear to have specifically targeted Resident 11, having administered him non-prescribed meds at least nine times.
- Resident 2
On January 8, 2019 paramedics also bagged Resident 2 in an ambulance en route from LHH to an acute care hospital, and administered a 2 mg dose of Narcan® to reverse the effects of an opioid overdose. Resident 2 almost suffered respiratory arrest and could have died. An acute care hospital MD (MD #8) reportedly spoke with LHH medical providers and were told LHH staff were investigating the case. MD #8 was so concerned about the care of Resident 2 that she kept the patient at the acute hospital for one week because the doctor didn’t want to send Resident 2 “to her death,” because the MD had “heard of several similar incidences at [LHH].”
On October 23, Troy Williams — who was brought in from SFGH as LHH’s Acting Director of Quality Management — testified to the Board of Supervisors GAO Committee, saying:
“There is evidence to support the possibility of those staff members bringing medications [in] from the outside. You know, there is some evidence to support that maybe they could have diverted it from Laguna Honda, but a lot of the things I’ve been privy to, it’s quite honestly probably medications that they brought [in] from the outside and were medicating patients with medications that were not prescribed.”
 Hogwash! The CDPH July 12 survey reported LHH’s Director of Pharmacy, Michelle Fouts, had told state inspectors that the meds appeared to have purloined by the fired nursing staff from patients who had been prescribed them, and was not likely the result of illegals drugs having been brought in from the outside.
Hogwash! The CDPH July 12 survey reported LHH’s Director of Pharmacy, Michelle Fouts, had told state inspectors that the meds appeared to have purloined by the fired nursing staff from patients who had been prescribed them, and was not likely the result of illegals drugs having been brought in from the outside.
During an interview on July 2] “The Director of Pharmacy (DOP) stated that LVN 1 was drugging Residents. The DOP also stated that LVN 1 most likely was taking patients medications to give to other patients. The DOP said that LVN 1 texted a picture to CNA 1 holding a bag of medications. The DOP believed that LVN 1 would take one patients’ medication and put them in a bag to later give other patients that were not prescribed these medications.
In an interview on 7 /3/19 at 3:00 PM the DOP stated that the medications in the bag were clearly from Laguna Honda Hospital.”
Scope and Severity of Patient Abuse at LHH
Table 2 shows LHH received five major deficiencies — all involving sub-standard care in long-term care facilities — in the CDPH July 12, 2019 survey, including the worst “L” finding, and received five additional lesser deficiencies during CDPH’s September 3 resurvey.
Table 2: CMS Substandard Care Deficiencies “Severity and Scope” Scale
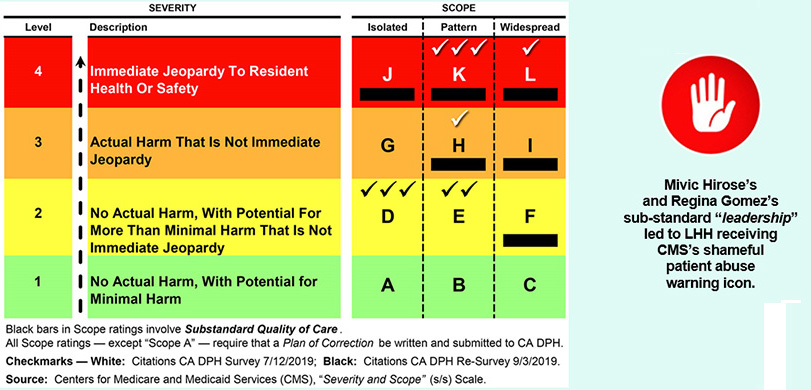
- Following CDPH’s initial July 12 survey, it imposed the highest severity-and-scope “L” finding for widespread violation of CMS F-Tag #607, which involves failure to develop or implement abuse and neglect policies.
 CDPH slapped LHH with three severity-and-scope “K” findings for patterns of F-Tag #583, which involves patient privacy and confidentiality of patient records; F-Tag #600, which involves failure to keep long-term care patients free from abuse and neglect; and F-Tag #605, for failing to ensure patients are kept free from “chemical restraints” (e.g., medicating patients with sedatives for staff convenience).
CDPH slapped LHH with three severity-and-scope “K” findings for patterns of F-Tag #583, which involves patient privacy and confidentiality of patient records; F-Tag #600, which involves failure to keep long-term care patients free from abuse and neglect; and F-Tag #605, for failing to ensure patients are kept free from “chemical restraints” (e.g., medicating patients with sedatives for staff convenience).
- CDPH also issued a severity-and-scope “H” finding for a pattern F-Tag #689, requiring that patients be kept free from accident and supervision hazards.
All five of the July 12 severity-and-scope findings involved sub-standard quality of care.
When CDPH returned for its follow-up re-survey conducted between September 3 and September 6, it slapped LHH with another five lesser citations that didn’t rise to the level of sub-standard care, but were still violations:
- CDPH also issued three severity-and-scope “D” findings for isolated incidents involving F-Tag #557, failure to treat patients with dignity and respect; F-Tag #607, for failure to develop and implement policies to prevent abuse and neglect; and F-Tag #689, requiring patients be kept free from accident and supervision hazards.
- CDPH issued two more severity-and-scope “E” pattern findings for F-Tag #600, for failure to keep patients free from abuse and neglect; and F-Tag #755, involving pharmacy services, and pharmacy records and procedures.
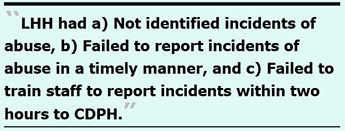 Of note, the 61-page CDPH July 12 survey report noted in three separate places that LHH had a) Not identified incidents of abuse, b) Failed to report incidents of abuse in a timely manner to CDPH, and c) Failed to train staff as “mandated reporters” to report incidents of abuse directly, and within two hours, to CDPH.
Of note, the 61-page CDPH July 12 survey report noted in three separate places that LHH had a) Not identified incidents of abuse, b) Failed to report incidents of abuse in a timely manner to CDPH, and c) Failed to train staff as “mandated reporters” to report incidents of abuse directly, and within two hours, to CDPH.
Unfortunately CDPH did not include in its July 12 report which LHH incidents — and how many — hadn’t been reported at all, or which incidents — and how many — were not reported in a timely manner, nor did CDPH report the dates on which specific incidents weren’t identified or the dates on which incidents were not reported in a timely manner, so we have no idea at this point just how far back the unreported events occurred.
 LHH’s “Leadership” Belatedly Fingered in Abuse Scandal
LHH’s “Leadership” Belatedly Fingered in Abuse Scandal
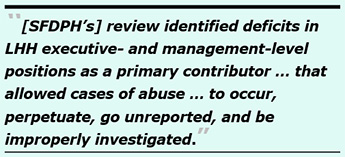
Four months after Breed’s June 28 press conference announcing the scandal, the San Francisco Board of Supervisors slowly got around to holding a hearing. During the Board’s Government Audit and Oversight (GAO) hearing on October 23, Supervisor Norman Yee asked whether LHH’s leadership had either ignored, or didn’t know about, the patient abuse scandal. Acting LHH CEO Margaret Rykowski — brought in from DPH to replace Hirose — responded, saying:
“[SFDPH’s] review … did identify deficits in executive- and management-level positions as a primary contributor … that allowed cases of abuse … to occur, perpetuate, go unreported, and be improperly investigated over extended periods of time. We’ve made initial steps [changing LHH’s] executive leadership, and will continue to make more, as needed.”
Rykowski didn’t elaborate on which leadership “deficits” were discovered.
During the GAO hearing, Rykowski asserted that LHH’s leadership “was made aware of the [abuse] incidents” in February 2019. That’s utter nonsense, when not wishful thinking. Mcshane knew of the drugging of patients problem a year earlier, in February 2018, and he should have made LHH’s entire leadership — and the Health Commission’s LHH-JCC — aware of the problem then, in order to thoroughly investigate the root cause of what was going on.
For his part, Troy Williams indicated “leadership creates and really sets the tone for the culture.” He added, “culture starts with leadership.”
The abuse scandal comes down, in part, to not having checks and balances on LHH’s leaders, including Hirose, Gomez, Valencia, and the Health Commissioners on the LHH-JCC, too. Supervisor Yee specifically noted that maybe the Health Commissioners didn’t ask the right questions. Williams tired to assert he didn’t know how the Commissioners would know about the problems unless Laguna Honda’s leadership knew about it and came forward with the information to the Health Commissioners. It’s clear LHH’s leadership may have kept the abuse problems away from the Health Commission.
 During the same GAO hearing, Supervisor Aaron Peskin asked whether it is true the terms of separation of the six nursing assistants apparently fired by May 6 include “the fact they can no longer access pensions.” As of November 22, that question hasn’t been answered. Peskin also asked whether the City Attorney could additionally sue the perpetrators for civil monetary penalties to help recover the City’s state and federal abuse-related fines.
During the same GAO hearing, Supervisor Aaron Peskin asked whether it is true the terms of separation of the six nursing assistants apparently fired by May 6 include “the fact they can no longer access pensions.” As of November 22, that question hasn’t been answered. Peskin also asked whether the City Attorney could additionally sue the perpetrators for civil monetary penalties to help recover the City’s state and federal abuse-related fines.
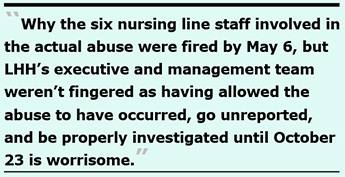
Why the six nursing line staff involved in the actual abuse were apparently fired by May 6, but LHH's executive and management team weren’t fingered as having allowed the abuse to have occurred, go unreported, and be properly investigated until October 23, is worrisome.
For that matter, since the six nursing staff were fired as early as May 6, why did it take Mayor Breed two months before staging her press conference on June 28?
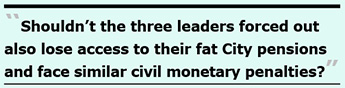 More worrisome is why the six perpetrators who were fired may lose their pensions and face civil monetary penalty (and criminal) lawsuits, but no questions were raised during the October 23 GAO hearing about whether the three leaders may face the same penalties. Shouldn’t the three leaders forced out also lose access to their fat City pensions and face similar civil monetary penalties for their failure to promptly report the abuse to the State?
More worrisome is why the six perpetrators who were fired may lose their pensions and face civil monetary penalty (and criminal) lawsuits, but no questions were raised during the October 23 GAO hearing about whether the three leaders may face the same penalties. Shouldn’t the three leaders forced out also lose access to their fat City pensions and face similar civil monetary penalties for their failure to promptly report the abuse to the State?
The Three Nursing Management Amigos
Even before Breed’s June 28 press conference, LHH CEO Mivic Hirose was forced to step down, and LHH’s Director of Quality Management was removed. The City tried to block release of the QM director’s name, claiming it was a “personnel matter,” but public records and a Google search easily revealed the name of the director — Regina Gomez, RN.
The two leaders were pushed out even before CDPH released it’s 61-page investigation July 12 survey report. The report revealed Hirose and Gomez were interviewed by CDPH investigators three times between May 29 and June 19 in the presence of a Deputy City Attorney and LHH’s Director of Nursing (DON). A Google search and public records revealed the DON was Madonna Valencia, RN.
Hirose, Gomez, and Valencia were also interviewed individually between May 29 and June 5. But Valencia wasn’t pushed out until October 7. It took four months before we learned that Valencia was also ousted. The three Nursing management amigos are not to be confused with Donald Trump’s and Rudy Giuliani’s three amigos: Kurt Volker, Gordon Sondland, and Rick Perry.
The executive- and management-level staff Rykowski was referring to who were eventually forced out — but handed soft landings in cushy positions — were, essentially, toadies. They are:
- Mivic Hirose, RN
Ms. Hirose has worked for DPH for 34 years, clearly long enough to have earned full vesting in her eventual pension.
She was first hired as a Medical-Surgical Staff Nurse at UC Davis Medical Center in 1985, and transferred to SFGH as a Medical Staff Nurse in the same year. She worked at SFGH for 14 years in medical-surgical, surgical/trauma intensive care, and discharge planning positions before becoming SFGH’s Medical/Surgical Nursing Director in 1999. Simultaneously, she held a three-year appointment between 1989 and 1992 at UCSF’s Renal Center as an Acute and Chronic Dialysis Nurse. In 1999 she transferred to LHH, as a co-Director of Nursing alongside Gayling Gee, the other Nursing Co-Director.
At the time she transferred to LHH, Mivic had no on-the-job experience in long-term care skilled nursing facilities, let alone in geriatric nursing.
In July 2006, Hirose engineered a coup, forcing Gee from being Co-Director of Nursing to being LHH’s Chief Operations Officer, leaving Hirose as the sole Chief Nursing Officer for three years until she was appointed as LHH’s CEO in 2009 following the death of John Kanaley.
When Hirose was pushed out as LHH’s CEO shortly before Breed’s June 28 press conference, Mivic was paid $309,215 in the fiscal year that ended on June 30, 2019. According to the City Controller’s Office after she was forced out and was assigned as an Informatics Clinical Nurse Specialist in DPH’s Information Technology department on its Clinical Informatics Team, she was paid $8,864 for the two-week payroll period ending October 18, which will translate to an annual salary of $230,464 if she manages to stay employed by DPH for another year, a significant $78,751 decrease in pay.
On the upside, if she chooses to retire, she will likely earn a $141,000 annual pension if she’s now age 58, or $180,219 if she’s age 62 or older, based on her reduced one-year salary. But if her pension formula is based on her average salary over her last three years of employment, as some union-represented employees get, she’ll earn an annual pension of between $157,110 if she’s 58 years old, or $200,751 if she’s 62 or older, or more.
As noted above, the illustration shown at the top of this article clearly shows LHH had celebrated Patient Safety Awareness Week April 11 through April 17, 2018. Hirose had to have known about that week-long patient safety “awareness” celebration, and had to have known that promoting a culture of patient safety was a core element of her job as CEO.
 Just four months after Hirose’s promotion to being LHH’s CEO in July 2009, Ms. Gee spoke out during a Health Commission meeting advocating to save LHH’s Adult Day Health Center program, using her First Amendment free-speech rights as a private citizen — rights for City employees protected by San Francisco’s Sunshine Ordinance. Hirose retaliated, telling Ms. Gee on a Friday to get out within 24 hours, being fired.
Just four months after Hirose’s promotion to being LHH’s CEO in July 2009, Ms. Gee spoke out during a Health Commission meeting advocating to save LHH’s Adult Day Health Center program, using her First Amendment free-speech rights as a private citizen — rights for City employees protected by San Francisco’s Sunshine Ordinance. Hirose retaliated, telling Ms. Gee on a Friday to get out within 24 hours, being fired.
Gayling cleared out her office Saturday, and retired the next day on November 22, 2009, four days before Thanksgiving Day. On Monday, nobody said a word about Gee’s forced ouster, although we were all shocked, as Gee undoubtedly was. After serving for 22 years at LHH, there was no going-away party for her — and no thanks for her dedicated services to the City, LHH, and its patients. Gee’s ouster was clearly retaliation for having exercised her First Amendment rights during a public meeting at which she had made clear before starting her testimony that she was speaking in her role as a private citizen, not in her role as an employee of LHH. It wasn’t the last time that Hirose engaged in retaliatory termination, since she was principally involved in wrongfully terminating Dr. Kerr in 2010.
Hirose tried to curry favor with DPH’s then-director, Dr. Mitch Katz, who wanted to turn LHH into a “Social Rehabilitation Facility for the Urban Poor.”
In 2004 Hirose, then LHH’s Director of Nursing, and my then-supervisor at LHH, Dr. Lisa Pascual, obtained a $50,000 grant from the California HealthCare Foundation (CHCF) to conduct a “social rehabilitation” research study under the title, “Enhancing Team Effectiveness to Improve Resident Function and Well-Being,” a misnomer if there ever was one. The “Leveraging Leadership” grants were available only to alumni of CHCF’s “Leadership Program.” Pascual was an alum of the Leadership Program’s 2001–2003 cohort. Pascual’s final cohort PPT presentation used the Wizard of Oz as a metaphor, somewhat apt to LHH’s wayward leadership style (there’s no place like home, and the Wizard behind the curtain is, indeed, a fraudster). Hirose tagged along in CHCF’s 2002–2004 leadership cohort. Neither seemed to have learned much about leadership from the two-year program.
The pair formed five sub-teams, by clinical specialty. When it came time for Pascual and Hirose to write up their final report to their funders at the end of the so-called grant, I had to polish the five PowerPoint presentations the five clinical teams had developed as their “scientific” conclusions. I was appalled by the PPT file the Nursing Team (including Valencia) turned in, because it mostly featured many Facebook-style photos of the Nurses in action at social and luncheon events, not any meaningful narrative of what their Nursing interventions had done to improve the social rehabilitation — let alone the care — of LHH’s residents.
 Rather than urge the Nursing Team as their proofreader and editor to include some data points (say “N =” and “n =”) as I had done for the other four sub-teams and disciplines, I chose not to say a word, and just let the Nursing team look as foolish as they liked. The grant-funded “research” contributed nothing to the scientific literature, or to patients’ well-being.
Rather than urge the Nursing Team as their proofreader and editor to include some data points (say “N =” and “n =”) as I had done for the other four sub-teams and disciplines, I chose not to say a word, and just let the Nursing team look as foolish as they liked. The grant-funded “research” contributed nothing to the scientific literature, or to patients’ well-being.
If Hirose had an ounce of cultural humility in her bones, she would resign in disgrace.
- Regina Gomez, RN
 Gomez was first hired into a position in LHH’s Quality Management Department on October 13, 1998. She was promoted from a Nurse Manager to a Nursing Supervisor on June 2, 2007, the same date that she was named as LHH’s Acting Director of Quality Management and later promoted to permanent director, where she has served for over a dozen years. As of this writing in 2019, she has been continuously employed in LHH's Quality Managemnt Department for 21 years, long enough to qualify for her eventually fat City pension.
Gomez was first hired into a position in LHH’s Quality Management Department on October 13, 1998. She was promoted from a Nurse Manager to a Nursing Supervisor on June 2, 2007, the same date that she was named as LHH’s Acting Director of Quality Management and later promoted to permanent director, where she has served for over a dozen years. As of this writing in 2019, she has been continuously employed in LHH's Quality Managemnt Department for 21 years, long enough to qualify for her eventually fat City pension.
Just before she was pushed out of LHH shortly before Breed’s June 28 press conference, Gomez was paid $278,193 in the fiscal year that ended on June 30, 2019.
As of September 27, all DPH would admit to was that Gomez had exercised her civil service rights to return to her former job classification as a Nursing Supervisor, and had been on a leave of absence since sometime in June. DPH claimed it could not provide additional information about which sub-department and facility Gomez had been transferred to and her working job title, because it would be “an invasion [of her] employee privacy.” DPH reportedly told the San Francisco Chronicle that Gomez was not expected to return from admin leave.
But according to the City Controller’s Office, she was paid $10,360 for the two week payroll period ending September 20, which would translate to an annual salary of $269,360 if she does return, a slight $8,833 decrease in pay.
Early on, Regina shared with some LHH staff that she had never been a bedside nurse doing direct patient care, having gone straight from nursing school into nursing administration. Clerical and secretarial water-cooler conversation wondered, “If it’s so important to have a nurse run QM, why choose a nurse who has never treated patients?” Her non-clinical background might have accounted for her managerial orientation, which was definitely not patient-centered.
More secretarial water-cooler conversations revealed that during a QM staff meeting in front of others, Gomez had berated one of her employees between 2007 and 2008 by saying, “When I tell you to do something, I expect you to do it immediately without any hesitation,” and for emphasis, had clapped her hands together making a rat-a-tat-tat sound, signaling “Chop-chop!” That was simply barbaric behavior from a senior manager. She was known to terrorize her subordinates, including secretarial staff.
Dr. Kerr and Dr. Rivero wrote a terrific article in the May 2015 Westside Observer, titled “Laguna Honda’s Falling Star,” referring to the Five-Star rating system for nursing facilities CMS first implemented in 2009. They reported LHH’s overall rating had been a two-star in 2010, rose to a three-star rating in 2011, captured a four-star rating in 2012, and somehow wrangled a five-star rating in 2013. It lost the fifth star in 2014, and as of October 15, 2018 — when Gomez was still at LHH — dropped to a two-star overall rating, where it remains. Unfortunately, the star ratings are suspect because they are based primarily on self-reporting, and LHH’s staff can minimize adverse events by under-reporting, or not reporting, which incidents are transmitted to CDPH or Medicare.
 The Health Inspections portion of the CMS rating system aren’t based on self-reporting. Instead, the Health Inspection star rating is scored independently by State inspectors following State surveys. As of October 2018, LHH’s Health Inspections score fell to a miserable one-star rating (Much Below Average) — on Ms. Gomez’s watch. A year later, LHH received CMS’s shameful patient abuse red icon.
The Health Inspections portion of the CMS rating system aren’t based on self-reporting. Instead, the Health Inspection star rating is scored independently by State inspectors following State surveys. As of October 2018, LHH’s Health Inspections score fell to a miserable one-star rating (Much Below Average) — on Ms. Gomez’s watch. A year later, LHH received CMS’s shameful patient abuse red icon.
DPH, the Health Commission, and its LHH-JCC should have known there were major problems under Gomez’s and Hirose’s leadership, long before the patient abuse scandal erupted eight months later in June 2019.
Kerr and Rivero reported:
“A former LHH analyst, who requested anonymity, told us, ‘Laguna administrators, charged with filing self-reports that should have been forthcoming, accurate and even regretful, were indeed adept at gaming the system’.”
They also reported that LHH had received inspection deficiencies in 2014 for failing to report patient-on-patient physical abuse to the State, not knowing such reports were legally required.
During the October GAO hearing, Mr. Williams also indicated there was a level of expertise in LHH’s Quality Management staff that was lacking in ability to be able to investigate things like this — the patient abuse scandal — as they came up. Williams didn’t specifically mention Gomez’s skills, or lack thereof, but he did indicate that culture starts with leadership, with the implication that the level of expertise that may have been lacking in the QM department involved Gomez’s leadership abilities.
LHH QM department had a policy that each patient ward in the hospital was required to submit Unusual Occurrence (UO) reports to Gomez’s staff to document unusual patient incidents. Each UO had to be promptly coded by her staff for the type and severity of the unusual incidents. By report, Gomez would fight and quibble with her staff to the last man standing over coding of the UO’s to try to lessen the severity of each UO report and which incidents were reported to the State. From more water-cooler conversations, Gomez and the then-Deputy City Attorney assigned to LHH potentially appeared to believe letters to the State were up to their discretion.
CDPH’s 61-page July 12 survey states on page 59 that LHH’s Medical Staff’s Performance Improvement and Patient Safety Committee is responsible for reviewing each UO report, a unique number is assigned to each UO, and the LHH Risk Management Nurse shall assure the required follow-up letters are sent and placed in the CDPH file.
 It is thought Regina may have cherry-picked choosing which of the UO incidents were actually reported to the State by jealously monitoring the codes assigned. In the end, that may be what Regina was ousted for, since the July 12 survey noted in three separate places that LHH had not identified incidents of abuse and had failed to report incidents of abuse in a timely manner to CDPH:
It is thought Regina may have cherry-picked choosing which of the UO incidents were actually reported to the State by jealously monitoring the codes assigned. In the end, that may be what Regina was ousted for, since the July 12 survey noted in three separate places that LHH had not identified incidents of abuse and had failed to report incidents of abuse in a timely manner to CDPH:
What Williams may not have known is that early on in her tenure, multiple LHH employees believed Gomez and her predecessors were the worst possible stewards of quality of care.
If Ms. Gomez had any inkling of what cultural humility is, she would immediately resign in disgrace.
- Madonna Valencia, RN
Valencia was hired as an RN on August 22, 1999, and promoted to being an LHH Nurse Manager on November 10, 2001. She eventually became the Nurse Manager of the Physical Medicine Rehabilitation Unit. She was eventually promoted to being LHH’s Director of Nursing (DON) on September 6, 2014. She’s also been at LHH for 20 years, long enough to qualify her for a fat City pension.
Valencia was paid $294,666 in the fiscal year that ended on June 30, 2019. After she was pushed out as LHH’s DON in October, she was paid $11,686 for the two week payroll period ending October 4, which would translate to an annual salary of $303,836, a slight raise of $9,170 annually — assuming she continues to work for a full year.
When I initially asked on October 17 whether she was still employed by DPH, which DPH entity she may now work in, or alternatively, whether she was also on a paid leave of absence, DPH initially indicated the next day that she had also exercised her civil service rights to retain employment by returning to her previous Nurse Manager job classification code, but DPH declined to indicate in which sub-department she had been transferred to, again claiming her unit assignment would not be disclosed under “employee privacy protections.”
 On October 29, I appealed indicating that to my knowledge, there is no valid “employee privacy protection” exemption in the California Public Records Act or case law authorizing withholding disclosure of what DPH sub-unit a public employee is assigned to, and asked again that the information be provided.
On October 29, I appealed indicating that to my knowledge, there is no valid “employee privacy protection” exemption in the California Public Records Act or case law authorizing withholding disclosure of what DPH sub-unit a public employee is assigned to, and asked again that the information be provided.
On November 1, DPH finally relented and indicated Madonna had been assigned to SFGH’s Care Coordination Team, but was currently on an unspecified type of leave apparently, since October 7.
Many people had been wondering why Madonna survived the first purge, when Mivic and Regina were forced out even before Breed’s initial June 28 press event with Grant Colfax and Supervisor Yee. I’ve read all three of the CDPH surveys, starting with the first 61-page July 12 survey, and have read the September 30 and October CMS notices imposing, and then increasing, the fines.
It’s not known when LHH’s Plan of Correction was presented to the Health Commission after it had been submitted to CDPH on July 15 (without having been presented first to the Health Commission beforehand) promising that LHH nurse managers would interview each of their subordinate nurses about “burn out” and concerns they may have had about their coworkers. CMS had imposed the initial $1 million fine on September 3 (less the 35% discount for not contesting the findings).
On September 30, CMS increased LHH’s initial fine by approximately $72,000 to $1.12 million (again, before adjusting downward for the 35% discount), and imposed the denial of CMS payments for new admissions. My public records request showed Acting CEO Margaret Rykowski notified LHH staff by letter on October 7 that Madonna had been forced out (although Rykowski worded it more diplomatically than I am here).
LHH had previously been warned twice that it faced denial of CMS payment for new admissions beginning September 18 if it didn’t get back into substantial compliance, and the September 6 CDPH survey found LHH had not achieved substantial compliance, in part because of the failure to conduct all nurse check-ins.
CDPH then did its 18-page September 6 initial re-survey, and found more deficiencies, including the failure to do the check-ins with nursing staff for “burn out.” It is not that LHH only did a “handful” of the nurse manager check-ins. The September 6 CDPH survey report stated three nursing units were chosen, apparently at random, and of 148 nurses only 35 had received the “check-ins.” That’s just 23.6% of the 148 nurses.
So, in the seven-day period between the fine increase on September 30 — or possibly between the September 6 re-survey that uncovered just 23.6% of the nurses had received the Plan of  Correction promised check-in — Rykowski and DPH must have decided by October 7 that Madonna’s head had to roll, too, in part because the denial of CMS payment for new admissions was in effect between September 18 and October 15, partly the result of Madonna’s “leadership” failures. That’s why, and when, Valencia was finally forced out.
Correction promised check-in — Rykowski and DPH must have decided by October 7 that Madonna’s head had to roll, too, in part because the denial of CMS payment for new admissions was in effect between September 18 and October 15, partly the result of Madonna’s “leadership” failures. That’s why, and when, Valencia was finally forced out.
Vivian Imperiale, who worked at LHH for ten years as its Vocational Rehabilitation Therapist, noted that although LHH’s Plan of Correction provided to CDPH claimed that nurse managers would do check-ins with each nursing staff member under them, they only did a handful. “Shouldn’t they have been doing check-in’s routinely with their staff members individually as part of their job duties as nurse managers? Isn’t that expected of senior managers? And isn’t that a given?” Imperiale asks, given that the State was breathing heavily down LHH’s neck and LHH’s status was swinging in the balance.
On October 30 (almost a month after Madonna was forced out), CMS issued an additional $4,290 penalty that was also reduced 35% to just $2,789.
There you have it: The patient abuse scandal involved the failure of nursing staff supervision under Valencia, and involved executive- and management-level failures by Hirose and Gomez. Good riddance to all three of them!
 History of LHH’s Leadership Problem Evolution
History of LHH’s Leadership Problem Evolution
Without putting too fine of a point on this, LHH’s leadership problems have had a long “colorful” history. It’s helpful to review that history.
Back in 2003 and 2004, then-Director of Public Health Mitch Katz instituted a disastrous “flow project” to discharge dangerous, robust behaviorally-challenged younger patients from SFGH into LHH, mixing them in with elderly vulnerable patients, many of whom had dementia’s, creating a volatile milieu for both patient populations. Katz did so by forcing successive changes to LHH’s Admissions Policy because he remained angry that LHH’s medical staff and hospital administrators had refused to accept and admit dangerous psychiatric patients from SFGH.
Flexing his biceps, Katz forced LHH’s Medical Director, Dr. Terry Hill, to resign, and eliminated Mary Louise Fleming’s position as LHH’s Director of Nursing. Katz also ousted LHH’s then Executive Administrator, Larry Funk — an at-will “exempt” employee. LHH’s then-Chief Operating Officer, Robert Christmas, offered himself for the CEO position. Katz declined, telling Christmas “you are too nice for the job.”
Katz appointed John Kanaley as Funk’s replacement in November 2004. Mr. Funk was the last LHH CEO to actually hold a Nursing Home Administrator license.
When news surfaced Funk had been forced out, 415 LHH staff — including nurses, certified nursing assistants, social workers, activity therapists, dietitians, physical therapists and occupational therapists, hospital volunteers, psychologists, and clerical and secretarial employees, among others — signed a petition to the then-president of the Health Commission, Edward Chow, MD urging that Funk be restored immediately to his position as CEO.
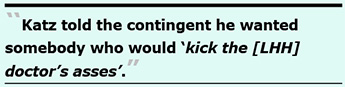 Another 32 members of LHH’s Medical Services Department of doctors and psychiatrists signed a separate petition to Dr. Katz and the full San Francisco Health Commission, including Dr. Chow, expressing their wholehearted support of Funk, and urging Katz to re-instate Funk as CEO. Within weeks of Kanaley’s appointment, a contingent of LHH’s high-level senior administrators met with Dr. Katz regarding concerns about Kanaley’s appointment and his lack of credentials, experience, and qualifications. Katz reportedly told the contingent it didn’t matter because he wanted somebody who would “kick the [LHH] doctor’s asses.”
Another 32 members of LHH’s Medical Services Department of doctors and psychiatrists signed a separate petition to Dr. Katz and the full San Francisco Health Commission, including Dr. Chow, expressing their wholehearted support of Funk, and urging Katz to re-instate Funk as CEO. Within weeks of Kanaley’s appointment, a contingent of LHH’s high-level senior administrators met with Dr. Katz regarding concerns about Kanaley’s appointment and his lack of credentials, experience, and qualifications. Katz reportedly told the contingent it didn’t matter because he wanted somebody who would “kick the [LHH] doctor’s asses.”
Kanaley’s prior job experience was in “facilities management,” not hospital administration. He had served for 14 years in facilities management in SFGH’s Plant Services Department. He had earned a master’s degree in public health in 2001 — just three years before being appointed LHH’s executive administrator — authoring a thesis involving evaluation of hazardous waste operations.
Many people believed Kanaley was sent to perform hazardous employee removal of LHH’s staff. Kanaley had no experience whatsoever running a skilled nursing facility, and certainly had no experience or training in running a 1,200-bed nursing home having approximately 1,500 employees.
Kanaley also forced out Cheryl Austin, LHH’s Medical Records Director, who sued alleging racial discrimination and retaliation.
Shortly after becoming CEO, Kanaley managed to oust Christmas in an unlitigated deal at unknown expense to the City, setting in motion Kanaley’s future purges of LHH staff. LHH staff quickly learned that Kanaley was in way over his head, unqualified, and was both paranoid and a bully.
Also within weeks of his appointment to LHH, Kanaley summoned Sister Miriam Walsh, Maria Rivero, MD (who previously served as LHH’s Medical Director but had stepped down to return to practicing medicine as LHH’s Admitting Ward doctor), and I into his office, one by one, seeking to silence our collective First Amendment right concerns about the safety and care of LHH’s patients. The three of us essentially told Kanaley “no deal,” but that didn’t stop him from pursuing us.
[Full Disclosure: When Dr. Rivero was LHH’s Medical Director, she made the hiring decision in May 1999 to hire me to work in the Rehabilitation Services Department following a final job interview.]
Following the protracted battle between LHH staff and Katz, and facing mounting political pressure, then-Mayor Gavin Newsom eventually ordered Katz to reinstate LHH’s admission policy to its pre-2004 level. That helped, but we continued advocating for patient safety.
The stress of his job as CEO may have contributed to Kanaley’s fatal heart attack on March 19, 2009. It’s not known if his paranoia and bullying were contributing causes of death.
LHH’s leadership problems extended to leadership of San Francisco’s Health Commission.
- Ed Chow and David Sanchez
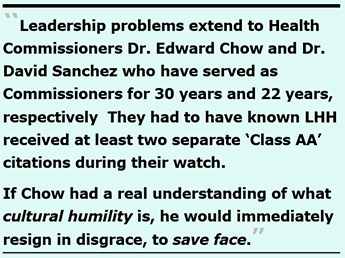 A key part of DPH’s leadership problems extends to Health Commissioners Dr. Edward Chow and Dr. David Sanchez who have served as Commissioners for 30 years and 22 years, respectively. Both men served repeatedly on the Commission’s LHH-Joint Conference Committee (LHH-JCC) that is charged, in part, with receiving LHH’s Quality Management reports.
A key part of DPH’s leadership problems extends to Health Commissioners Dr. Edward Chow and Dr. David Sanchez who have served as Commissioners for 30 years and 22 years, respectively. Both men served repeatedly on the Commission’s LHH-Joint Conference Committee (LHH-JCC) that is charged, in part, with receiving LHH’s Quality Management reports.
Sanchez resigned from the Health Commission in April 2019. Chow, who has served for 30 years on the Health Commission, should also resign, since he — and Sanchez — had served on the LHH-JCC repeatedly as its chairperson multiple times. Both men should have been aware of LHH’s quality management problems. They had to have known LHH had received at least two separate “Class AA” citations during their watch on the Health Commission.
If Dr. Chow had a real understanding of what cultural humility is, he would immediately resign in disgrace, to save face.
Fear of Retaliation Drove Silence
During the Board of Supervisors October 23 GAO hearing, Troy Williams bemoaned LHH’s lack of a culture of safety. He testified:
“I think this is a very important piece to this. One of the things we learned as a part of our investigation is that there was a culture of silence. These things were able to go on undetected for years. And, you know, what we’ve learned is that people were afraid to report. Retaliations — specifically, we heard a lot about these specific individuals involved, that there was some fear of them and retaliation from them. … I think that is something that is really important, because leadership creates and really sets the tone for the culture.”
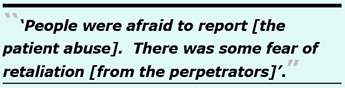 No kidding, Troy. While not diminishing the likelihood that some employees were afraid of peer-to-peer retaliation from low-level Licensed Vocational Nurses (LVN’s) and Certified Nursing Assistants (CNA’s), the greater fear of retaliation that drove the culture of silence was from senior hospital administrators.
No kidding, Troy. While not diminishing the likelihood that some employees were afraid of peer-to-peer retaliation from low-level Licensed Vocational Nurses (LVN’s) and Certified Nursing Assistants (CNA’s), the greater fear of retaliation that drove the culture of silence was from senior hospital administrators.
In December 2004, one Laguna Honda Hospital doctor shared with me:
“The only time [LHH’s] administration addresses [patient] safety issues is when it gets sued or cited [by state or federal agencies investigating patient abuse]. Whuzzup?”
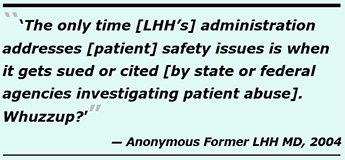 The same doctor remembered being told in the early 2000’s that if she reported patient-on-patient physical or verbal abuse due to inappropriate admissions and inadequate staff supervision on her ward of dementia patients, that there was no whistleblower protections for LHH doctors. That appears to have led to the 2014 inspection citations for failing to report the patient-on-patient abuse to CDPH, which Gomez may not have known was legally required.
The same doctor remembered being told in the early 2000’s that if she reported patient-on-patient physical or verbal abuse due to inappropriate admissions and inadequate staff supervision on her ward of dementia patients, that there was no whistleblower protections for LHH doctors. That appears to have led to the 2014 inspection citations for failing to report the patient-on-patient abuse to CDPH, which Gomez may not have known was legally required.
Given Hirose’s well-known history of retaliation against Gayling Gee and Dr. Kerr, and perhaps others, the fear of retaliation from Nursing leadership is far higher. How can Mr. Williams, Ms. Rykowski, and Supervisor Yee not have known this?
 Unanswered Questions
Unanswered Questions
Many key questions remain. CANHR asked on September 11: What’s being done to bring the perpetrators to justice? What’s the Police Department — specifically its Special Victims Unit — doing? Why hasn’t the State Attorney General’s Elder Abuse Unit filed charges against the perpetrators? And why hasn’t CDPH denounced the abuse and publicly released its findings?
 After all, the drugging of patients with unprescribed opioids was first detected and reported to LHH’s Medical Director, Dr. Michael Mcshane, as early as February 26, 2018 by doctors at other hospitals where five patients had been transported with life-threatening conditions, including respiratory arrest. Mcshane replied the same day that an internal investigation was underway at LHH. Did Mcshane ever conclude that internal investigation? Why hasn’t he been forced out, too?
After all, the drugging of patients with unprescribed opioids was first detected and reported to LHH’s Medical Director, Dr. Michael Mcshane, as early as February 26, 2018 by doctors at other hospitals where five patients had been transported with life-threatening conditions, including respiratory arrest. Mcshane replied the same day that an internal investigation was underway at LHH. Did Mcshane ever conclude that internal investigation? Why hasn’t he been forced out, too?
In his terrific November 2019 Westside Observer article, former LHH physician Dr. Derek Kerr — wrongfully terminated in June 2010 in retaliation for whistleblowing — asked what had happened with investigations by LHH’s physician-run Medical Quality Improvement Committee and its Performance Improvement and Patient Safety Committee, since both committees appear to have fallen victim to, and have offered, silence. That mirrors LHH’s pandemic culture of silence. Kerr noted “Ignoring root causes [of problems at LHH] is a structural component of LHH’s Culture of Silence.”
Personally, I wonder why the San Francisco District Attorney’s Office hasn’t announced criminal charges in this scandal. After all, aren’t District Attorneys supposed to focus on the victims of crimes and the impacts of the crimes on them in a timely manner?
 Hirose, Gomez, Valencia, Chow, Sanchez, and Mcshane all had to have known the December 2016 “Class AA” citation’s two-year period hadn’t ended. Is that why the patient abuse wasn’t reported promptly to the State?
Hirose, Gomez, Valencia, Chow, Sanchez, and Mcshane all had to have known the December 2016 “Class AA” citation’s two-year period hadn’t ended. Is that why the patient abuse wasn’t reported promptly to the State?
On, November 19 CDPH responded to a records request saying “CDPH cannot comment on an ongoing investigation.” Why has CDPH’s investigation dragged on from at least May 29 to November 19 without conclusion? The answer may be as CANHR reported on October 24: CDPH’s backlog of over 17,000 cases of open complaints and facility reports of abuse.
That backlog may have contributed to Dennis Herrera having been able to wrangle the reduction of the 2016 “Class AA” citation down to a “Class A” violation. How many citations in other abuse cases were also reduced because of CDPH’s backlog of investigations?
What DPH and LHH may be ignoring at their own peril is that there will always be employees who have eyes and ears, and despite the culture of silence the truth will eventually come out. Hopefully, when future employees see something, they’ll say something now that Hirose’s and Gomez’s reigns of terror are finally over.
Watch this space.
Monette-Shaw is a columnist for San Francisco’s Westside Observer newspaper, and a member of the California First Amendment Coalition (FAC) and the ACLU. He operates stopLHHdownsize.com. Contact him at monette-shaw@westsideobserver.com.
Top
 Ironically, also on October 23, the Centers for Medicare and Medicaid Services (CMS) rolled out its new warning icon on its Nursing Home Compare website to alert consumers about long-term care facilities at which patient abuse had been uncovered. LHH was promptly hit with the new icon by CMS somewhere between October 23 and November 30, 2019. Thanks, “leaders”!
Ironically, also on October 23, the Centers for Medicare and Medicaid Services (CMS) rolled out its new warning icon on its Nursing Home Compare website to alert consumers about long-term care facilities at which patient abuse had been uncovered. LHH was promptly hit with the new icon by CMS somewhere between October 23 and November 30, 2019. Thanks, “leaders”!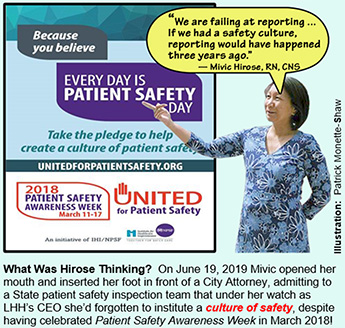 Printer-friendly PDF file
Printer-friendly PDF file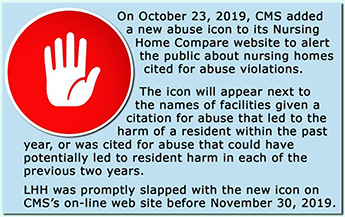 Toss in the nonsensical word-salad pabulum from Health Commissioner Dr. Ed Chow about a totally unrelated problem involving cultural humility, and you know there’s a real problem of culture and a likelihood the conspiracy of silence will prevail. Some observers believe the problems at LHH definitely involved a conspiracy of silence across multiple departments, including its Nursing Department and its Medical Services Department.
Toss in the nonsensical word-salad pabulum from Health Commissioner Dr. Ed Chow about a totally unrelated problem involving cultural humility, and you know there’s a real problem of culture and a likelihood the conspiracy of silence will prevail. Some observers believe the problems at LHH definitely involved a conspiracy of silence across multiple departments, including its Nursing Department and its Medical Services Department. Patient Abuse Scandal Erupts
Patient Abuse Scandal Erupts Mcshane replied to the UCSF doctor that an internal investigation into the case was underway. Nine months later, the same patient was again transferred on October 26, 2018 to an acute care hospital because of mental status changes as a result of other medications which had also not been prescribed. A second LHH patient who had also stopped breathing and had respiratory arrest was transported to an acute care hospital on January 8, 2018. A different acute hospital doctor had been told LHH’s staff was investigating the second case. So, Colfax should have known that rather than starting an investigation in February 2019, LHH had purportedly been investigating for over a year. Colfax should also have known that a third patient wrongly administered opioids he had not been prescribed died on September 2, 2018.
Mcshane replied to the UCSF doctor that an internal investigation into the case was underway. Nine months later, the same patient was again transferred on October 26, 2018 to an acute care hospital because of mental status changes as a result of other medications which had also not been prescribed. A second LHH patient who had also stopped breathing and had respiratory arrest was transported to an acute care hospital on January 8, 2018. A different acute hospital doctor had been told LHH’s staff was investigating the second case. So, Colfax should have known that rather than starting an investigation in February 2019, LHH had purportedly been investigating for over a year. Colfax should also have known that a third patient wrongly administered opioids he had not been prescribed died on September 2, 2018. Mivic should have known after having been either LHH’s Co-Director or sole Director of Nursing for 10 years, and after having been LHH’s CEO for an additional decade, that submitting patient abuse reports to CDPH within two hours was not optional, but a mandatory, ministerial requirement to promote a culture of safety. What was she thinking making such a ridiculous admission? There should have been a culture of reporting, along with a culture of patient safety. Furthermore, LHH’s
Mivic should have known after having been either LHH’s Co-Director or sole Director of Nursing for 10 years, and after having been LHH’s CEO for an additional decade, that submitting patient abuse reports to CDPH within two hours was not optional, but a mandatory, ministerial requirement to promote a culture of safety. What was she thinking making such a ridiculous admission? There should have been a culture of reporting, along with a culture of patient safety. Furthermore, LHH’s 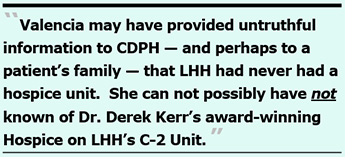 Valencia’s name was also uncovered from a simple Google search.
Valencia’s name was also uncovered from a simple Google search.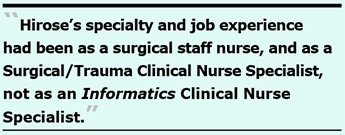 Problem is, a “
Problem is, a “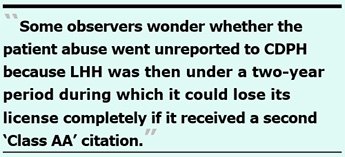 “Class AA” Violations
“Class AA” Violations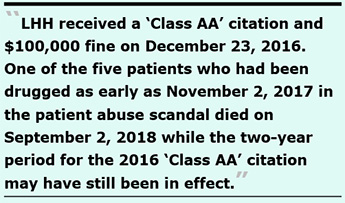 LHH had received a “Class AA” citation and a $100,000 fine on December 23, 2016. As early as November 2, 2017 — within the first year — one of the five patients who had been drugged tested positive for Methadone he hadn’t been prescribed. He was drugged eight additional times with different opioids through August 2018. He died on September 2, 2018 while the two-year period for the 2016 “Class AA” citation was still in effect. It’s probable LHH may end up receiving another “Class AA” citation for his death thanks, in part, to Hirose’s “leadership.”
LHH had received a “Class AA” citation and a $100,000 fine on December 23, 2016. As early as November 2, 2017 — within the first year — one of the five patients who had been drugged tested positive for Methadone he hadn’t been prescribed. He was drugged eight additional times with different opioids through August 2018. He died on September 2, 2018 while the two-year period for the 2016 “Class AA” citation was still in effect. It’s probable LHH may end up receiving another “Class AA” citation for his death thanks, in part, to Hirose’s “leadership.” After the Health Commission approved the settlement, it then took the Board of Supervisors until November 5, 2019 to pass an Ordinance on second reading agreeing to pay the $100,000 fine, and ostensibly approve the settlement. It’s not known on what date Mayor Breed may have approved the settlement.
After the Health Commission approved the settlement, it then took the Board of Supervisors until November 5, 2019 to pass an Ordinance on second reading agreeing to pay the $100,000 fine, and ostensibly approve the settlement. It’s not known on what date Mayor Breed may have approved the settlement. Because the lawsuit isn’t “officially” fully closed, it’s not clear on what date, if any, CDPH’s two-year period for “Class AA” violations may have stopped, or whether CDPH’s two-year clock had remained ticking at the time Patient 11 died in September 2018. Thanks, Mivic!
Because the lawsuit isn’t “officially” fully closed, it’s not clear on what date, if any, CDPH’s two-year period for “Class AA” violations may have stopped, or whether CDPH’s two-year clock had remained ticking at the time Patient 11 died in September 2018. Thanks, Mivic!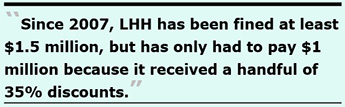 Fines and Penalties Against LHH
Fines and Penalties Against LHH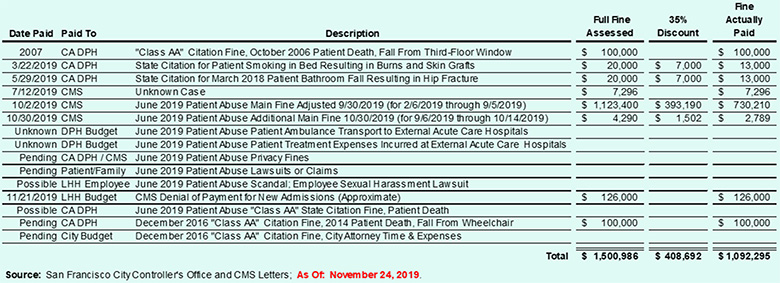
 What this suggests is that although there were fines imposed for patients wrongly administered opioid-level meds they had not been prescribed, no fines may have been imposed for other patients who were prescribed meds that they may never have received. Again, not to put too fine a point on this, harm was caused to both patients drugged without orders, and more harm was caused to patients who may not have received their pain control meds. Didn’t Hirose — or CDPH, SFDPH, the Health Commission, or the Board of Supervisors — notice this glaring problem?
What this suggests is that although there were fines imposed for patients wrongly administered opioid-level meds they had not been prescribed, no fines may have been imposed for other patients who were prescribed meds that they may never have received. Again, not to put too fine a point on this, harm was caused to both patients drugged without orders, and more harm was caused to patients who may not have received their pain control meds. Didn’t Hirose — or CDPH, SFDPH, the Health Commission, or the Board of Supervisors — notice this glaring problem? On October 23, the Board of Supervisors were advised (below) that additional fines against the hospital are still expected because privacy fines take more time, and are typically steep.
On October 23, the Board of Supervisors were advised (below) that additional fines against the hospital are still expected because privacy fines take more time, and are typically steep. On February 26, 2018 an MD at the acute care hospital concerned about Resident 6’s presenting circumstances e-mailed LHH Medical Director, Dr. Michael Mcshane, reporting the u-tox results. According to the state survey report, Mcshane reportedly replied indicating that an internal investigation was underway at LHH. The acute care hospital MD also e-mailed the final comprehensive toxicology report to Mcshane on March 5, 2018.
On February 26, 2018 an MD at the acute care hospital concerned about Resident 6’s presenting circumstances e-mailed LHH Medical Director, Dr. Michael Mcshane, reporting the u-tox results. According to the state survey report, Mcshane reportedly replied indicating that an internal investigation was underway at LHH. The acute care hospital MD also e-mailed the final comprehensive toxicology report to Mcshane on March 5, 2018. Resident 11 was viewed by the LVN and CNA as a “difficult” resident and may have been administered non-prescribed meds “to put him to sleep” to render him less difficult “for their convenience.” The State survey did not report a specific date on which Resident 11 was transferred to an acute care hospital. Resident 11 did have a physician’s order for weekly urine toxicology screens. Resident 11 first tested positive for Methadone on November 2, 2017 and tested positive eight more times between January 17 and August 6, 2018 for Morphine, Methadone, and Oxycodone. One of the tox screens identified both Oxycodone and Morphine; another tox screen identified both Morphine and Methadone.
Resident 11 was viewed by the LVN and CNA as a “difficult” resident and may have been administered non-prescribed meds “to put him to sleep” to render him less difficult “for their convenience.” The State survey did not report a specific date on which Resident 11 was transferred to an acute care hospital. Resident 11 did have a physician’s order for weekly urine toxicology screens. Resident 11 first tested positive for Methadone on November 2, 2017 and tested positive eight more times between January 17 and August 6, 2018 for Morphine, Methadone, and Oxycodone. One of the tox screens identified both Oxycodone and Morphine; another tox screen identified both Morphine and Methadone.  Hogwash! The CDPH July 12 survey reported LHH’s Director of Pharmacy, Michelle Fouts, had told state inspectors that the meds appeared to have purloined by the fired nursing staff from patients who had been prescribed them, and was not likely the result of illegals drugs having been brought in from the outside.
Hogwash! The CDPH July 12 survey reported LHH’s Director of Pharmacy, Michelle Fouts, had told state inspectors that the meds appeared to have purloined by the fired nursing staff from patients who had been prescribed them, and was not likely the result of illegals drugs having been brought in from the outside.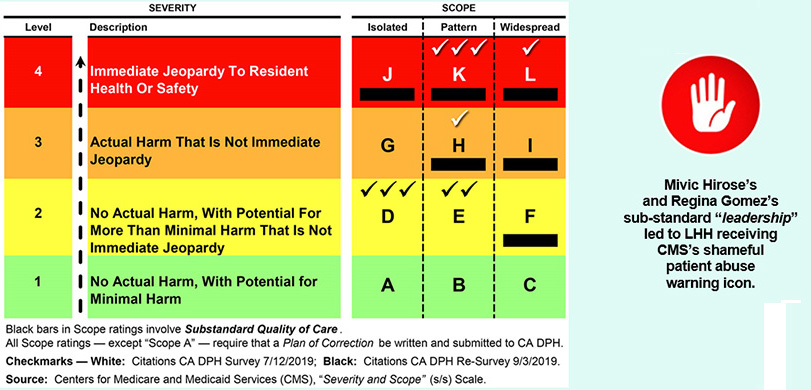
 CDPH slapped LHH with three severity-and-scope “K” findings for patterns of F-Tag #583, which involves patient privacy and confidentiality of patient records; F-Tag #600, which involves failure to keep long-term care patients free from abuse and neglect; and F-Tag #605, for failing to ensure patients are kept free from “chemical restraints” (e.g., medicating patients with sedatives for staff convenience).
CDPH slapped LHH with three severity-and-scope “K” findings for patterns of F-Tag #583, which involves patient privacy and confidentiality of patient records; F-Tag #600, which involves failure to keep long-term care patients free from abuse and neglect; and F-Tag #605, for failing to ensure patients are kept free from “chemical restraints” (e.g., medicating patients with sedatives for staff convenience). Of note, the 61-page CDPH July 12 survey report noted in three separate places that LHH had a) Not identified incidents of abuse, b) Failed to report incidents of abuse in a timely manner to CDPH, and c) Failed to train staff as “mandated reporters” to report incidents of abuse directly, and within two hours, to CDPH.
Of note, the 61-page CDPH July 12 survey report noted in three separate places that LHH had a) Not identified incidents of abuse, b) Failed to report incidents of abuse in a timely manner to CDPH, and c) Failed to train staff as “mandated reporters” to report incidents of abuse directly, and within two hours, to CDPH. LHH’s “Leadership” Belatedly Fingered in Abuse Scandal
LHH’s “Leadership” Belatedly Fingered in Abuse Scandal During the same GAO hearing, Supervisor Aaron Peskin asked whether it is true the terms of separation of the six nursing assistants apparently fired by May 6 include “the fact they can no longer access pensions.” As of November 22, that question hasn’t been answered. Peskin also asked whether the City Attorney could additionally sue the perpetrators for civil monetary penalties to help recover the City’s state and federal abuse-related fines.
During the same GAO hearing, Supervisor Aaron Peskin asked whether it is true the terms of separation of the six nursing assistants apparently fired by May 6 include “the fact they can no longer access pensions.” As of November 22, that question hasn’t been answered. Peskin also asked whether the City Attorney could additionally sue the perpetrators for civil monetary penalties to help recover the City’s state and federal abuse-related fines.  More worrisome is why the six perpetrators who were fired may lose their pensions and face civil monetary penalty (and criminal) lawsuits, but no questions were raised during the October 23 GAO hearing about whether the three leaders may face the same penalties. Shouldn’t the three leaders forced out also lose access to their fat City pensions and face similar civil monetary penalties for their failure to promptly report the abuse to the State?
More worrisome is why the six perpetrators who were fired may lose their pensions and face civil monetary penalty (and criminal) lawsuits, but no questions were raised during the October 23 GAO hearing about whether the three leaders may face the same penalties. Shouldn’t the three leaders forced out also lose access to their fat City pensions and face similar civil monetary penalties for their failure to promptly report the abuse to the State? Just four months after Hirose’s promotion to being LHH’s CEO in July 2009, Ms. Gee spoke out during a Health Commission meeting advocating to save LHH’s Adult Day Health Center program, using her First Amendment free-speech rights as a private citizen — rights for City employees protected by San Francisco’s Sunshine Ordinance. Hirose retaliated, telling Ms. Gee on a Friday to get out within 24 hours, being fired.
Just four months after Hirose’s promotion to being LHH’s CEO in July 2009, Ms. Gee spoke out during a Health Commission meeting advocating to save LHH’s Adult Day Health Center program, using her First Amendment free-speech rights as a private citizen — rights for City employees protected by San Francisco’s Sunshine Ordinance. Hirose retaliated, telling Ms. Gee on a Friday to get out within 24 hours, being fired.  Rather than urge the Nursing Team as their proofreader and editor to include some data points (say “N =” and “n =”) as I had done for the other four sub-teams and disciplines, I chose not to say a word, and just let the Nursing team look as foolish as they liked. The grant-funded “research” contributed nothing to the scientific literature, or to patients’ well-being.
Rather than urge the Nursing Team as their proofreader and editor to include some data points (say “N =” and “n =”) as I had done for the other four sub-teams and disciplines, I chose not to say a word, and just let the Nursing team look as foolish as they liked. The grant-funded “research” contributed nothing to the scientific literature, or to patients’ well-being. Gomez was first hired into a position in LHH’s Quality Management Department on October 13, 1998. She was promoted from a Nurse Manager to a Nursing Supervisor on June 2, 2007, the same date that she was named as LHH’s Acting Director of Quality Management and later promoted to permanent director, where she has served for over a dozen years. As of this writing in 2019, she has been continuously employed in LHH's Quality Managemnt Department for 21 years, long enough to qualify for her eventually fat City pension.
Gomez was first hired into a position in LHH’s Quality Management Department on October 13, 1998. She was promoted from a Nurse Manager to a Nursing Supervisor on June 2, 2007, the same date that she was named as LHH’s Acting Director of Quality Management and later promoted to permanent director, where she has served for over a dozen years. As of this writing in 2019, she has been continuously employed in LHH's Quality Managemnt Department for 21 years, long enough to qualify for her eventually fat City pension. The Health Inspections portion of the CMS rating system aren’t based on self-reporting. Instead, the Health Inspection star rating is scored independently by State inspectors following State surveys. As of October 2018, LHH’s Health Inspections score fell to a miserable one-star rating (Much Below Average) — on Ms. Gomez’s watch. A year later, LHH received CMS’s shameful patient abuse red icon.
The Health Inspections portion of the CMS rating system aren’t based on self-reporting. Instead, the Health Inspection star rating is scored independently by State inspectors following State surveys. As of October 2018, LHH’s Health Inspections score fell to a miserable one-star rating (Much Below Average) — on Ms. Gomez’s watch. A year later, LHH received CMS’s shameful patient abuse red icon. It is thought Regina may have cherry-picked choosing which of the UO incidents were actually reported to the State by jealously monitoring the codes assigned. In the end, that may be what Regina was ousted for, since the July 12 survey noted in three separate places that LHH had not identified incidents of abuse and had failed to report incidents of abuse in a timely manner to CDPH:
It is thought Regina may have cherry-picked choosing which of the UO incidents were actually reported to the State by jealously monitoring the codes assigned. In the end, that may be what Regina was ousted for, since the July 12 survey noted in three separate places that LHH had not identified incidents of abuse and had failed to report incidents of abuse in a timely manner to CDPH: On October 29, I appealed indicating that to my knowledge, there is no valid “employee privacy protection” exemption in the California Public Records Act or case law authorizing withholding disclosure of what DPH sub-unit a public employee is assigned to, and asked again that the information be provided.
On October 29, I appealed indicating that to my knowledge, there is no valid “employee privacy protection” exemption in the California Public Records Act or case law authorizing withholding disclosure of what DPH sub-unit a public employee is assigned to, and asked again that the information be provided. Correction promised check-in — Rykowski and DPH must have decided by October 7 that Madonna’s head had to roll, too, in part because the denial of CMS payment for new admissions was in effect between September 18 and October 15, partly the result of Madonna’s “leadership” failures. That’s why, and when, Valencia was finally forced out.
Correction promised check-in — Rykowski and DPH must have decided by October 7 that Madonna’s head had to roll, too, in part because the denial of CMS payment for new admissions was in effect between September 18 and October 15, partly the result of Madonna’s “leadership” failures. That’s why, and when, Valencia was finally forced out. History of LHH’s Leadership Problem Evolution
History of LHH’s Leadership Problem Evolution Another 32 members of LHH’s Medical Services Department of doctors and psychiatrists signed a separate petition to Dr. Katz and the full San Francisco Health Commission, including Dr. Chow, expressing their wholehearted support of Funk, and urging Katz to re-instate Funk as CEO. Within weeks of Kanaley’s appointment, a contingent of LHH’s high-level senior administrators met with Dr. Katz regarding concerns about Kanaley’s appointment and his lack of credentials, experience, and qualifications. Katz reportedly told the contingent it didn’t matter because he wanted somebody who would “kick the [LHH] doctor’s asses.”
Another 32 members of LHH’s Medical Services Department of doctors and psychiatrists signed a separate petition to Dr. Katz and the full San Francisco Health Commission, including Dr. Chow, expressing their wholehearted support of Funk, and urging Katz to re-instate Funk as CEO. Within weeks of Kanaley’s appointment, a contingent of LHH’s high-level senior administrators met with Dr. Katz regarding concerns about Kanaley’s appointment and his lack of credentials, experience, and qualifications. Katz reportedly told the contingent it didn’t matter because he wanted somebody who would “kick the [LHH] doctor’s asses.”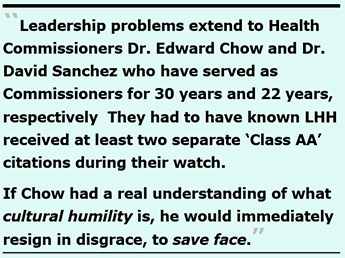 A key part of DPH’s leadership problems extends to Health Commissioners Dr. Edward Chow and Dr. David Sanchez who have served as Commissioners for 30 years and 22 years, respectively. Both men served repeatedly on the Commission’s LHH-Joint Conference Committee (LHH-JCC) that is charged, in part, with receiving LHH’s Quality Management reports.
A key part of DPH’s leadership problems extends to Health Commissioners Dr. Edward Chow and Dr. David Sanchez who have served as Commissioners for 30 years and 22 years, respectively. Both men served repeatedly on the Commission’s LHH-Joint Conference Committee (LHH-JCC) that is charged, in part, with receiving LHH’s Quality Management reports.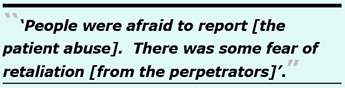 No kidding, Troy. While not diminishing the likelihood that some employees were afraid of peer-to-peer retaliation from low-level Licensed Vocational Nurses (LVN’s) and Certified Nursing Assistants (CNA’s), the greater fear of retaliation that drove the culture of silence was from senior hospital administrators.
No kidding, Troy. While not diminishing the likelihood that some employees were afraid of peer-to-peer retaliation from low-level Licensed Vocational Nurses (LVN’s) and Certified Nursing Assistants (CNA’s), the greater fear of retaliation that drove the culture of silence was from senior hospital administrators.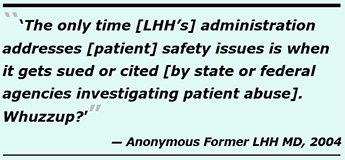
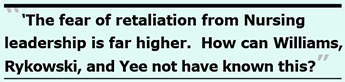 Unanswered Questions
Unanswered Questions After all, the drugging of patients with unprescribed opioids was first detected and reported to LHH’s Medical Director, Dr. Michael Mcshane, as early as February 26, 2018 by doctors at other hospitals where five patients had been transported with life-threatening conditions, including respiratory arrest. Mcshane replied the same day that an internal investigation was underway at LHH. Did Mcshane ever conclude that internal investigation? Why hasn’t he been forced out, too?
After all, the drugging of patients with unprescribed opioids was first detected and reported to LHH’s Medical Director, Dr. Michael Mcshane, as early as February 26, 2018 by doctors at other hospitals where five patients had been transported with life-threatening conditions, including respiratory arrest. Mcshane replied the same day that an internal investigation was underway at LHH. Did Mcshane ever conclude that internal investigation? Why hasn’t he been forced out, too? Hirose, Gomez, Valencia, Chow, Sanchez, and Mcshane all had to have known the December 2016 “Class AA” citation’s two-year period hadn’t ended. Is that why the patient abuse wasn’t reported promptly to the State?
Hirose, Gomez, Valencia, Chow, Sanchez, and Mcshane all had to have known the December 2016 “Class AA” citation’s two-year period hadn’t ended. Is that why the patient abuse wasn’t reported promptly to the State?