 July 16, 2025
July 16, 2025A Crisis of In-County Skilled Nursing Bed Capacity
 July 16, 2025
July 16, 2025
A Crisis of In-County Skilled Nursing Bed Capacity
Laguna Honda Hospital’s Lost 120-Beds Spin Control
$53.6 Million on Consultant Contracts.
$230 Million in Lost Medi-Cal Revenue.
$8.2 Million in Fines, Penalties and Lawsuit Settlements.
$8 Million in Five Employee’s Salaries.
Then City Abandons Saving LHH’s 120 Beds?
by Patrick Monette-Shaw
The loss of 120 beds at Laguna Honda Hospital for the indefinite foreseeable future — at least three-and-a-half years remaining in the Trump administration, plus perhaps another four to eight years should Democrats fail to win the White House in 2028 — involves a lot of gaslighting, when not pure spin control, from the Federal government.
 It doesn’t help that San Franciscans may also be being gaslit by our local media, and San Francisco’s Department of Public Health and its Health Commission.
It doesn’t help that San Franciscans may also be being gaslit by our local media, and San Francisco’s Department of Public Health and its Health Commission.
The loss of LHH’s 120 beds was a predictable — but entirely avoidable — result of, and directly related to, LHH’s decades-long “culture of silence,” that led to the loss of having a “culture of safety,” that lead to a “culture of neglect” — all driven by an ugly history of a “culture of mismanagement.” All driven by City managers and employees lacking experience, training, or licensure in running a skilled nursing facility, exacerbated by performance failures of Laguna Honda’s “governing body,” San Francisco’s Health Commission.
A San Francisco Chronicle article on July 24 and an SFist article on July 25 didn’t describe adequately what led to LHH’s 120-bed loss, and failed to examine in depth the vacuous reasoning behind the Federal government’s denial of the City’s waiver to save the beds, that are critically needed — now.
 For its part, SFist asserted LHH had “reputational fallout” from two patient illicit drug overdoses in 2019, so CMS is punishing LHH for bureaucratic reasons. SFist also reported LHH was frustrated CMS had alleged LHH had 276 incidents of non-compliance since its recertification in 2023, but had received only six citations for the 276 incidents. SFist’s 499-word article grossly understated the problem. Neither the Chronicle nor SFist mentioned LHH has had at least 290 “scope-and-severity” citations from inspections by state and federal inspectors, approximately 2,586 Facility-Reported Incidents (FRI’s) since 2016, and by LHH’s own (but undercounted) admission, at least 49 verified deficiencies between 2024 and 2025 alone.
For its part, SFist asserted LHH had “reputational fallout” from two patient illicit drug overdoses in 2019, so CMS is punishing LHH for bureaucratic reasons. SFist also reported LHH was frustrated CMS had alleged LHH had 276 incidents of non-compliance since its recertification in 2023, but had received only six citations for the 276 incidents. SFist’s 499-word article grossly understated the problem. Neither the Chronicle nor SFist mentioned LHH has had at least 290 “scope-and-severity” citations from inspections by state and federal inspectors, approximately 2,586 Facility-Reported Incidents (FRI’s) since 2016, and by LHH’s own (but undercounted) admission, at least 49 verified deficiencies between 2024 and 2025 alone.
As for the Chronicle, it reported largely the same nonsense in its skimpy 522-word article (as if the Chron couldn’t afford to buy more ink), but tossed in for good measure that indeed, state inspectors had identified “moderate to very serious” deficiencies at LHH in 2022. Both news outlets repeated the City’s spin control that pursuing legal action to fight CMS’s second waiver denial would “be costly, time consuming, and unlikely to yield a timely or favorable result.”
Both media outlets severely understated the severity of LHH’s actual sustained deficiencies, fines, financial administrative penalties, lawsuit settlements, and costs of San Francisco City Attorney time and expenses. And both news articles neglected to mention that LHH had very, very serious deficiencies, including 27 “Immediate Jeopardy” and “Actual Harm” citations since 2019, and fines and administrative penalties long before 2022 and 2023, dating back to the patient sexual abuse scandal at LHH in 2019.
Although my Westside Observer colleague, Theresa Palmer, MD wrote a terrific piece in the Observer in July, her article also didn’t wade into historical details that need to be preserved about this disaster.
 This article seeks to thoroughly preserve that historical record.
This article seeks to thoroughly preserve that historical record.
LHH’s Waiver Request Denied — Again
LHH dragged its feet before submitting its waiver request to save 120 of its skilled nursing facility beds. Had the waiver been submitted in 2023 or in early 2024, it would have stood a chance of being approved long before the Donald Trump Administration descended in January 2025, and we’d still have LHH’s 120 beds.
Part of the delay was because LHH had gaslit the public that the Centers for Medicare and Medicaid Services (CMS) had initially claimed that no more than two residents could share a common bathroom. Subsequently, LHH claimed CMS’ rationale had later morphed into asserting that because LHH had been decertified in April 2022, that LHH suddenly had to comply with a 2016 rule change not allowing more than two residents per bedroom for skilled nursing facilities seeking (new) CMS certification. LHH eventually finally flatly refuted that interpretation.
A big part of the delay, obviously, was it shamefully took LHH 26 months during decertification to retrain its obdurate and entrenched managers and nursing staff on how to run LHH as a skilled nursing facility. Both LHH’s CEO, and its hired consultant HSAG, had written in late 2022 after decertification that LHH staff still threatened to jeopardize passing recertification inspections, including such minor things as not properly donning and doffing PPE (personal protective equipment) like face masks and gloves.
Another part of the delay in filing the waiver application was because after LHH gained recertification in the Medi-Cal program from the California Department of Public Health (CPDH) in August 2023 and from CMS in June 2024, LHH delayed resuming patient admissions waiting to ensure significant changes and improvements made over the past two years were being sustained by LHH’s staff. LHH resumed admissions painfully slowly, deliberately, and methodically.
It wasn’t until five months later, on November 27, 2024 that LHH submitted its first waiver request, after LHH thought its staff were sustaining regulatory compliance improvements consistently, and LHH asserted it finally understood how to address CMS’s concerns as best as possible. CMS rejected the first waiver request in January 2025.
 Based on verbal conversations LHH ostensibly had with CMS to address CMS’ concerns, when LHH finally got around to resubmitting its revised waiver request to CMS on April 11, 2025 LHH rightly stated that because Laguna Honda was certified prior to 2016 and offers rooms that are even larger than required, CMS’ rulemaking in 2016 didn’t apply to LHH, because the 2016 final rule change had clearly stated, “existing facilities with larger rooms are effectively grandfathered into compliance” with Code of Federal Regulations §49083.90(d)(1) about the maximum number of patients per room.
Based on verbal conversations LHH ostensibly had with CMS to address CMS’ concerns, when LHH finally got around to resubmitting its revised waiver request to CMS on April 11, 2025 LHH rightly stated that because Laguna Honda was certified prior to 2016 and offers rooms that are even larger than required, CMS’ rulemaking in 2016 didn’t apply to LHH, because the 2016 final rule change had clearly stated, “existing facilities with larger rooms are effectively grandfathered into compliance” with Code of Federal Regulations §49083.90(d)(1) about the maximum number of patients per room.
Concerns about the CMS’ proposed rulemaking in an October 4, 2016 Federal Register extract included comments from skilled nursing facility providers, including their misunderstanding of the revised rules on page 9 (68695), which stated:
“Comment: A number of commenters responded to our request for comments in ways that suggest misunderstandings of either current requirements or the proposed requirements. Notable misconceptions include the [mistaken] belief that existing facilities would have to limit occupancy to two residents per room, even if that would reduce bed count.”
In response to the commenter’s concerns, the Federal Register’s clarifying response also stated on page 9:
“The ‘‘two persons per room’’ requirement applies only to those facilities that receive approval to be constructed or reconstructed, or are newly certified after this rulemaking. Existing facilities with larger rooms are effectively grandfathered into compliance.”
In its revised waiver request, LHH rightly noted CMS’ insistence LHH was not grandfathered to the pre-2016 rule change was an arbitrary and capricious interpretation of the Federal Register’s clarification on this issue.
LHH’s April 11 resubmitted waiver request rightly discussed that CMS’ 2016 final rule did not define the term “newly certified,” and the U.S. Department of Health and Human Services’ (HHS) commentary in both the proposed and final rules made clear that the rulemaking’s intent was to apply the rule prospectively, not retrospectively to existing facilities that were then currently certified in 2016 to participate in Medicare and/or Medicaid.
CMS has essentially been quibbling about the difference between “newly certified” vs. “re-certified.” When LHH submitted its waiver requests in both November 2024 and April 2025, it was seeking to be re-certified, not newly certified. CMS’s denial of LHH’s 120-bed waiver request amounted to an end-run around the intent of CMS and HHS in 2016 that facilities with more than two residents per room were grandfathered, and, therefore, exempt from the revised rulemaking.
 It’s almost as if CMS itself had misunderstood the Federal Register’s explanation of the intent of the rulemaking in 2015 and 2016, with CMS creatively ignoring LHH’s long-standing certification as an “existing facility” and that LHH was essentially seeking re-certification as a grandfathered facility, not seeking first-time certification.
It’s almost as if CMS itself had misunderstood the Federal Register’s explanation of the intent of the rulemaking in 2015 and 2016, with CMS creatively ignoring LHH’s long-standing certification as an “existing facility” and that LHH was essentially seeking re-certification as a grandfathered facility, not seeking first-time certification.
In its July 7 denial letter, CMS suddenly raised a new issue about the number of deficiencies, addressed below, that essentially amounts to more gaslighting from the Trump Administration.
More CMS Gaslighting Spin Control
In its July 7, 2025 rejection letter, CMS mischaracterizes the controlling federal regulation by adding:
“CMS may permit variations of the various resident bedroom requirements listed at 42 C.F.R. §483.90(e)(1)(i) and (ii) in individual cases where a facility can demonstrate that the variance is in accordance with the special needs of the residents and will not adversely affect resident health and safety.”
First, CMS ignores the fact that §483.90(e)(3) specifically authorizes the California Department of Public Health (CDPH) to grant LHH the 120-bed waiver request, because LHH is also a “nursing facility,” an issue LHH addressed in its March 11 resubmitted waiver request. CMS’ claim it is the “sole arbiter” of this decision is just more gaslighting.
Second, CMS ignored the sound rationale in LHH’s April 11 waiver resubmission in which LHH adequately addressed the issue of whether LHH’s residents’ health and safety would be adversely affected, by well documenting that it would not.
§483.90(e)(1)(i) stipulates there can be no more than four residents per bedroom, except that facilities “newly certified” by CMS after November 28, 2016 can have no more than two residents per bedroom. For its part, 42 C.F.R. §483.90(e)(1) (ii), simply states bedrooms must measure at least 80 square feet per resident in multiple resident bedrooms, and at least 100 square feet in single resident bedrooms. LHH documented its larger rooms exceed minimum square footage requirements.
CMS went on in its July 7 letter by lurching into deceitful spin control, writing:
“Review of the text of § 483.90(e)(3) demonstrates that CMS has the discretion to permit variances on a limited basis for an individual bedroom as needed to best assist a specific resident to attain their highest practicable state, with that variance expiring once the specific resident was no longer present.”
 Although §483.90(e)(3) does stipulate that in “individual cases” a facility must be able to demonstrate that the variation to the number of residents per room are in accordance with the special needs of the residents and must not adversely affect residents’ health and safety, CMS wrongly asserts §483.90(e)(3) includes language allowing CMS to withdraw the “variance” to the rule (the waiver), or that the waiver will expire, when a given resident is no longer there.
Although §483.90(e)(3) does stipulate that in “individual cases” a facility must be able to demonstrate that the variation to the number of residents per room are in accordance with the special needs of the residents and must not adversely affect residents’ health and safety, CMS wrongly asserts §483.90(e)(3) includes language allowing CMS to withdraw the “variance” to the rule (the waiver), or that the waiver will expire, when a given resident is no longer there.
There’s nothing in §483.90(e) that provides any such thing about the waiver expiring when a given resident moves on. In addition, it is thought that the clause “in individual cases” was intended by CMS’ 2016 Federal Register rulemaking change to refer to individual facilities may apply for a waiver request, not that it applies to individual patients.
It appears CMS raised this gaslighting claim for the first time in its July 7 denial letter, and didn’t give LHH and our City Attorney an opportunity to rebut and challenge this newly raised nonsense beforehand in LHH’s formal written waiver resubmission on April 11.
Our local media mentioned nothing about any of this gaslighting.
 CMS Moved the Goalpost
CMS Moved the Goalpost
Unfortunately, when CMS denied LHH’s second waiver application on July 7, 2025 CMS suddenly switched the goalposts, pulling a bait-and-switch and largely abandoning its previous objections about the number of patients that could share a bathroom, or share bedrooms. In its place, CMS introduced a new concern apparently not previously raised in verbal conversations with LHH officials so they could address those concerns before submitting LHH’s revised written appeal.
CMS pulled out of its spin control rabbit hat, that LHH had over 1,600 allegations of non-compliance, including allegations of abuse, neglect, and resident rights violations, along with facility-reported incidents (FRI’s) and anonymous complaints in the six years prior to LHH’s decertification in April 2022. The “six years prior” included the three years before LHH’s patient sexual abuse scandal in 2019.
For good measure, CMS tossed in that LHH had had hundreds of more allegations of violations — without quantifying a precise actual number — following LHH’s re-entry into Medicaid (Medi-Cal) in December 2023 following its Medi-Cal recertification in August 2023, and then its Medicare recertification in June 2024 as the new primary basis for CMS’ second denial of LHH’s 120-bed waiver request on July 7.
Moving the goalpost and switching to the number of incidents that have occurred at LHH obviously deprived LHH of being able to address this formally and beforehand in its April 11 resubmitted waiver request.
That said, LHH faces a hard time refuting CMS’ allegations of abuse and number of incidents, because of LHH’s long history of problems.
LHH Gaslights Its Deficiencies
 Fully a week after receiving CMS’ July 7 denial letter via e-mail — e-mailed to Troy Williams, of all people, rather to Roland Pickens, CEO the of San Francisco Health Network (SFHN) under whose signature LHH’s April11 waiver requested had been submitted, or to Daniel Tsai, San Francisco’s Director of Public Health — LHH responded to members of the public with gaslighting of its own on July 14 in what appears to be a carefully worded press release, when not spin control. Troy Williams hadn’t even been included as a courtesy copy recipient of Pickens’ April 11 waiver request, although Tsai was. [Note: Williams was the lead author of the 2019 “LHH 60-Day Reform Plan” that became a complete failure.]
Fully a week after receiving CMS’ July 7 denial letter via e-mail — e-mailed to Troy Williams, of all people, rather to Roland Pickens, CEO the of San Francisco Health Network (SFHN) under whose signature LHH’s April11 waiver requested had been submitted, or to Daniel Tsai, San Francisco’s Director of Public Health — LHH responded to members of the public with gaslighting of its own on July 14 in what appears to be a carefully worded press release, when not spin control. Troy Williams hadn’t even been included as a courtesy copy recipient of Pickens’ April 11 waiver request, although Tsai was. [Note: Williams was the lead author of the 2019 “LHH 60-Day Reform Plan” that became a complete failure.]
It’s not known whether LHH or the City Attorney have formally responded in writing to CMS yet.
LHH’s press release claimed CMS had mischaracterized LHH’s regulatory compliance, asserting that since Laguna Honda’s recertification in the Medicare Program in December 2023 LHH had received hundreds of allegations of non-compliance, including allegations of abuse, neglect, and resident rights violations. LHH quibbled about CMS having included both pre-2022 decertification reports and anonymous complaints not verified through formal survey findings, asserting that only six of 276 incident reports since December 2023 resulted in an actual deficiency. [LHH had significantly more than just 276 incidents!]
As if to justify, or refute, CMS’ assertion LHH had had over 1,600 incidents dating back to 2016, the July 14 press release also lamely asserted:
“Compared to other large skilled nursing facilities in California (299 beds or more), Laguna Honda ranks in the middle tier for reported incidents and well below the median for survey deficiencies. This reinforces that Laguna Honda’s performance is consistent with sector norms.”
But the press release failed to note — perhaps hoping the public wouldn’t remember — that LHH’s large facility employs a corresponding much larger  contingent of Nursing staff than othernursing facilities, in part because it’s a municipally-funded facility having generous salaries and pension plans. LHH’s contingent of 768 Nursing staff should have been better able to prevent the larger number of facility-reported incidents — particularly since its Nursing employees had remained at full staffing levels, even though its patient census had dropped by 40% during its decertification while still racking up incident reports. Surely LHH and its governing Health Commission must know that CMS and CDPH are well aware of LHH’s much larger Nursing staff.
contingent of Nursing staff than othernursing facilities, in part because it’s a municipally-funded facility having generous salaries and pension plans. LHH’s contingent of 768 Nursing staff should have been better able to prevent the larger number of facility-reported incidents — particularly since its Nursing employees had remained at full staffing levels, even though its patient census had dropped by 40% during its decertification while still racking up incident reports. Surely LHH and its governing Health Commission must know that CMS and CDPH are well aware of LHH’s much larger Nursing staff.
This sin of omission is nothing more than creative gaslighting via excluding relevant information.
 CMS had not specifically mentioned that LHH had had 276 incidents since December 2023 in its July 7 denial letter. It’s essentially a magic number LHH pulled out of thin air on July 14.
CMS had not specifically mentioned that LHH had had 276 incidents since December 2023 in its July 7 denial letter. It’s essentially a magic number LHH pulled out of thin air on July 14.
While Laguna Honda vigorously disputes CMS’ mischaracterization of its performance, it is nonetheless somewhat true.
LHH’s press release does state that the City will not be appealing CMS’ denial or pursuing litigation at this time. It says that while Laguna Honda and SFDPH strongly disagree with CMS’s decision, LHH now makes the strategic choice not to pursue legal action, because it would be “costly, time-consuming, and unlikely to yield a timely or favorable result—especially given CMS’s broad discretion and the current political climate” in Washington.
It’s unclear whether San Francisco’s Board of Supervisors or San Francisco’s full Health Commission were even consulted about this before SFDPH decided not to pursue litigation now.
The press release asserts local health departments like SFDPH must focus on protecting the broader system of care in the face of ongoing federal and state threats to millions of dollars in other Medicaid funding San Francisco depends upon. LHH’s press release claimed that instead of litigation, LHH and the City are prioritizing proactive efforts to expand skilled nursing capacity across the system and continuing to engage with CMS and the State about potential “alternative pathways.”
To date, we haven’t heard what specific “proactive efforts” SFDPH currently has underway, if any.
Also on July 14, LHH’s CEO, Diltar Sidhu sent a memo addressed to all LHH staff, essentially reiterating what LHH’s press release had outlined. Sadly, Sidhu’s letter to staff contained an error, because he asserted that while CMS had denied LHH’s “initial” waiver request [the first denial dated in January 2025], that LHH had resubmitted a “renewed” waiver application in December 2024, rather than correctly listing April 11 as the actual date of LHH’s second waiver resubmission.
And on July 14, LHH released a comparative analysis it had quickly cobbled together after receiving CMS’ July 7 denial of LHH’s waiver request. LHH’s comparative analysis is where it gaslit, claiming only six of 276 incident reports since December 2023 resulted in an actual deficiency. Indeed, LHH’s analysis clearly stated on pages 3 and 4 that between January 2024 and June 2025, Laguna Honda Hospital (LHH) had a total of 267 incidents and during the same period had a total of 49 deficiencies. LHH’s “new math” somehow converted its admission of 49 deficiencies down to just six.
[Note: LHH’s press release cited 276 incidents since December 2023, but its statistical analysis document cited 267 incidents, suggesting LHH couldn’t keep its statistics straight.]
Another problem is, LHH’s gaslighting analysis essentially compared apples to oranges: The analysis clearly states: “Analysis
assumes full resident census for California facilities and considers the average census for LHH.” I’m no statistician, but comparing the full census of other facilities to LHH’s “average” census sounds distinctly like lying with numbers using apples and oranges, by fiddling with the denominator.
As well, the data labels for LHH in the bar charts in the analysis use the number 649 (rather than LHH’s 769 licensed beds). But LHH hasn’t had an average census of 649 for well over three years. Indeed, LHH’s average monthly census in 2024 was just 425 residents, not 649. I was taught in high school that increasing the numerator by 200 (the average number of patients from 425 to 649) compared to the number of incidents will skew the rates-per-1,000 patients LHH’s analysis relied on, artificially lowering the rate-per-1,000 incidents.
The Westside Observer’s former columnist, Lou Barberini — a trained CPA — has noted: “When a San Francisco agency reports in percentage terms rather than actual [raw] numbers, you can be assured they are hiding something.”
 Regulatory Non-Compliance History
Regulatory Non-Compliance History
Although LHH is attempting to minimize its long history of deficiencies, citations, and “Immediate Jeopardy” and “Actual Harm” citations, both pre- and post-decertification in April 2022, LHH’s gaslighting won’t work because its non-compliance history comes from multiple sources — primarily from CDPH survey inspection reports, and LHH’s own data presented monthly to San Francisco’s Health Commission.
One source is data gleaned by tracking Form 2567 inspection reports by the California Department of Public Health (CDPH) “scope and severity” citations levied against LHH between 2019 and 2025.
That scope-and-severity data clearly shows that since LHH’s patient sexual abuse scandal surfaced in 2019 under former LHH CEO Mivic Hirose (who was then belatedly promptly let go), LHH has racked up at least 10 “Immediate Jeopardy” citations from CDPH, plus an additional 17 “Actual Harm” citations. There’s no minimizing those 27 citations. In addition, LHH received 257 citations that had the potential for causing patients more than just minimal harm.
Indeed, after LHH’s decertification in April 2022, LHH was hit with 5 of the 10 “Immediate Jeopardy” citations, and 12 of the 17 “Actual Harm” citations, even as LHH was scrambling mightily to save its sinking ship and spending millions in expense. Worse, LHH racked up five of the 17 “Actual Harm” citations after it was recertified in the Medi-Cal program in August 2023, but before being Medicare recertified in June 2024.
 Another source includes data gleaned from monthly “Regulatory Affairs Reports” LHH has presented to LHH’s “governing body,” the San Francisco Health Commission.
Another source includes data gleaned from monthly “Regulatory Affairs Reports” LHH has presented to LHH’s “governing body,” the San Francisco Health Commission.
A first view of the monthly data shows that of the 704 FRI’s LHH was required to report to CDPH since 2022 (not the mere 267 incidents LHH claimed in its July 14 press release), there were 27 “Disease Outbreak” FRI’s, 28 “Adverse Events,” 10 “Potential Privacy Breaches,” and at least 223 “Resident-to-Resident” abuse FRI’s, among others. And there were 134 “Anonymous Complaints” in addition to the 704 FRI’s. And following 76 survey inspection site visits from CDPH over those four years, LHH was required to submit at least 32 “Plans of Correction,” which typically are required only after receiving actual deficiencies.
A second view of the data suggests LHH had at least 1,857 Facility Reported Incidents (FRI’s) and anonymous complaints LHH reported to the Health Commission between 2019 and June 2025. But after adjusting to account for the 971 FRI’s in the “Regulatory Affairs Reports” for just three of years of data before LHH’s decertification, compared to the “over 1,600 allegations” over six years before LHH’s decertification CMS asserted in its July 7, 2025 denial of LHH’s waiver request, it suggests there were potentially an additional 729 FRI’s that LHH may have reported to CDPH.
 That brings the total number of FRI’s to 2,586 in the 10-year period between 2016 and 2025. Twenty-six hundred FRI’s suggests LHH indeed had an excessive number of incidents reported by the facility dating back to 2016, despite LHH’s gaslighting there were only 276 incidents and merely six deficiencies since December 2023.
That brings the total number of FRI’s to 2,586 in the 10-year period between 2016 and 2025. Twenty-six hundred FRI’s suggests LHH indeed had an excessive number of incidents reported by the facility dating back to 2016, despite LHH’s gaslighting there were only 276 incidents and merely six deficiencies since December 2023.
Another source of data comes from reports LHH’s external consultant, Health Services Advisory Group (HSAG), had published in nine “Root Cause Analysis” reports between December 1, 2022 and July 27, 2023, summarizing its work as the consultant CMS required LHH hire as a “Quality Improvement Expert” in June 2022, that identified 168 different root cause problems underlying LHH’s mismanagement that led to LHH’s decertification in April 2022.
 The root case problems are summarized in HSAG’s “Action Plan Final Summary” report, in descending number of root causes, stratified by the “foundational” root cause category, including the quality of care LHH provided its residents and development of care plans, since a large percentage of LHH’s deficiencies and citations across the years had involved substandard level-of-care violations.
The root case problems are summarized in HSAG’s “Action Plan Final Summary” report, in descending number of root causes, stratified by the “foundational” root cause category, including the quality of care LHH provided its residents and development of care plans, since a large percentage of LHH’s deficiencies and citations across the years had involved substandard level-of-care violations.
In addition, HSAG published seven “Monthly Monitoring Reports” between February 10, 2023 and August 10, 2023 analyzing LHH’s progress in implementing 960 remedial “Action Plan” corrective action “milestones” uncovered during HSAG’s thorough “Root Cause Analysis” investigations. The 960 corrective actions signaled the severity of LHH’s problems.
 HSAG’s “Action Plan Final Summary” report dated November 9, 2023 noted that even after LHH had become Medi-Cal recertified in August 2023, of the 960 action plan remedial actions, fully 298 (31%) required the QIE to step in and revise the milestone corrective actions, because LHH staff were still not adequately applying and performing “critical thinking skills” in how to implement the corrective actions. Disturbingly, of 107 milestones in the “Comprehensive Care Plans and Quality of Care” foundational root case category, HSAG had to revise 49 of the 107 (46%), and HSAG had to revise 65 of the 157 (41%) in the separate “Quality of Care” foundational category. The two Care Plans and Quality of Care categories combined totaled 264 of the 960 “milestones,” roughly 27.5% of the corrective actions necessary.
HSAG’s “Action Plan Final Summary” report dated November 9, 2023 noted that even after LHH had become Medi-Cal recertified in August 2023, of the 960 action plan remedial actions, fully 298 (31%) required the QIE to step in and revise the milestone corrective actions, because LHH staff were still not adequately applying and performing “critical thinking skills” in how to implement the corrective actions. Disturbingly, of 107 milestones in the “Comprehensive Care Plans and Quality of Care” foundational root case category, HSAG had to revise 49 of the 107 (46%), and HSAG had to revise 65 of the 157 (41%) in the separate “Quality of Care” foundational category. The two Care Plans and Quality of Care categories combined totaled 264 of the 960 “milestones,” roughly 27.5% of the corrective actions necessary.
HSAG concluded that the data presented indicated LHH was not sustaining “Action Plan” deliverable metrics, even after almost a year-and-a-half into HSAG’s work to bring LHH staff up into sustained regulatory compliance.
Despite LHH’s extensive gaslighting, these data sources clearly document LHH’s long noncompliance history and its many deficiencies.
Tsai’s and Chow’s July 14 Remarks
A partial verbatim transcript extract from the July 14, 2025 LHH-JCC meeting at which the announcement was made that CMS had denied LHH’s 120-bed waiver request for a second time was extremely disturbing. The transcript includes extensive comments made by San Francisco’s Director of Public Health, Daniel Tsai, and Health Commissioner Edward, Chow, MD.
During the 7/14/2025 LHH-JCC meeting, Director Tsai indicated that the City — presumably including the Mayor and Citty Attorney, with or without the approval of San Francisco’s Board of Supervisors — had decided to cave in and buckle to the bullies running the Donald Trump administration, and not pursue filing a lawsuit at this time to compel CMS to approve LHH’s 120-bed waiver request, even though protecting LHH’s skilled nursing beds is part of the continuum of care for San Francisco’s, most vulnerable elderly and disabled residents who rely on Medi-Cal for skilled nursing facility level of care.
Tsai said, in part:
“We are not conceding on the merits of our arguments [in our revised April 11 appeal] … But we are not intending at this point to pursue further appeals or [legal] actions. Just to be very wise about where and how we’re engaging with the Federal government, given the magnitude of cuts that are coming all around us at this point and that we need to be prepared to fight.”
That seems to contradict Tsai’s earlier statements during an earlier April 14, 2025 LHH-JCC meeting — after explicitly stating San Francisco needs more skilled nursing facility beds — that:
“… we said in the [April 11 waiver appeal] letter very clearly that from a legal standpoint, we think the Federal government needs to grant us this waiver for the 120 beds, and we outlined the legal reasons why.”
 Tsai effectively said on July 14 that despite having a very strong case to purse legally, that the City had decided between April and July to throw in the towel, and abandon, however temporarily, saving LHH’s 120 critically needed beds.
Tsai effectively said on July 14 that despite having a very strong case to purse legally, that the City had decided between April and July to throw in the towel, and abandon, however temporarily, saving LHH’s 120 critically needed beds.
Tsai also stated that CMS had made clear, apparently only in verbal discussions off-line, that the waiver request was “the last stop on the bus” and CMS was the sole arbiter of the decision claiming it was not delegable to the State of California at CDPH. That’s patently untrue, first, because LHH cited in its April 11 resubmitted appeal to CMS that Federal regulations allow in the case of a nursing facility CDPH can grant a variance to the 2016 two-person per room rule.
And second, the April 11 waiver appeal letter also stated on page 7, that as late as January 1, 2025 LHH had met with CMS staff, who agreed that LHH meets the variance requirements, and granting the waiver wouldn’t adversely affect LHH residents’ health. Despite LHH now meeting the variance requirements, CMS is still punishing LHH anyway.
This is another example of the Trump Administration getting away with simply moving the goal posts.
For his part, Chow said that in the face of the hundreds of millions of dollars in Medicaid funding cuts the State of California is facing, he agreed that Tsai’s conclusion not to pursue litigation to save LHH’s 120 beds makes sense. Chow asserted the priority at the moment is that its very important “we don’t fight too many battles on too many fronts, and it’s important to pick the battles carefully to [‘protect’] the most vulnerable areas so patients who do need care are able to get it.”
 Chow’s gaslighting lamely implied LHH was fortunate to be recertified at all. He actually stated San Francisco should be pleased that LHH is even able to have 500-plus beds at LHH. His meandering reply that LHH would even have 500 beds does not inspire confidence about the City ever remembering in the future to pursue submitting another waiver request to get LHH’s 120 beds back, as if Chow couldn’t recall or calculate that LHH losing 120 of its beds still leaves 649 — not 500 — SNF beds at LHH. Chow’s comments San Franciscans should accept having even “500-plus” beds at LHH, is deeply offensive, because there are patients now who need SNF care in-county, but aren’t able to get it, as Chow himself should know as a Health Commissioner.
Chow’s gaslighting lamely implied LHH was fortunate to be recertified at all. He actually stated San Francisco should be pleased that LHH is even able to have 500-plus beds at LHH. His meandering reply that LHH would even have 500 beds does not inspire confidence about the City ever remembering in the future to pursue submitting another waiver request to get LHH’s 120 beds back, as if Chow couldn’t recall or calculate that LHH losing 120 of its beds still leaves 649 — not 500 — SNF beds at LHH. Chow’s comments San Franciscans should accept having even “500-plus” beds at LHH, is deeply offensive, because there are patients now who need SNF care in-county, but aren’t able to get it, as Chow himself should know as a Health Commissioner.
San Francisco’s City Attorney should pursue litigation now to save LHH’s 120 beds. After all, those are largely Medicaid beds that serve the vulnerable elderly who are part of other vulnerable San Franciscans facing loss of additional Medicaid funding Director Tsai is rightly worried about also losing!
The idea that the City Attorney can only focus on fighting to preserve hundreds of millions in Federal government revenue the City rightly fears it will lose from Trump’s cuts in Medicaid reimbursement for vulnerable safety-net patients in other programs — and abandon fighting to save Laguna Honda’s 120 beds, which yield approximately $32.6 million annually in Medicare and Medi-Cal revenue reimbursement each year — is somewhat bonkers. After all, over a three-and-a-half-year period, LHH will lose approximately $114.1 million in Medicare funding from losing 120 of its beds, which is desperately needed to help pay the salaries of LHH’s 768 budgeted Nursing staff positions in various job classifications.
$300.5 Million Decertification Costs Subset
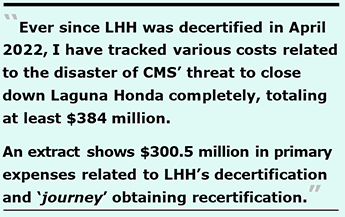
Ever since LHH was decertified in April 2022, I have tracked various costs related to the disaster of CMS’ threat to close down Laguna Honda completely. Those costs now total at least $384 million, but it’s an ongoing work still in progress.
Here is an extract of $300.5 million in primary expenses related to LHH’s decertification and “journey” toward obtaining recertification. The table tracks costs of external consultants still under contract to LHH and SFDPH; fines, penalties, and legal settlement costs against LHH; lost Medi-Cal revenue; and salary costs of five SFDPH staff who were largely responsible for LHH’s decertification. Brief caveats are in order.
One chart summarizing the $53.6 million in costs for external consultant shows HSAG is still working on a contract worth $10 million through the end of July 2029, to monitor and ensure LHH is sustaining compliance  with Federal nursing home regulations following its full recertification in June 2024. That work, and HSAG’s additional “mock inspection surveys” at LHH and LHH’s “organizational assessments,” are now largely being kept secret and confined to closed-door sessions during Health Commission meetings.
with Federal nursing home regulations following its full recertification in June 2024. That work, and HSAG’s additional “mock inspection surveys” at LHH and LHH’s “organizational assessments,” are now largely being kept secret and confined to closed-door sessions during Health Commission meetings.
Another chart shows that LHH has racked up $8 million in fines and penalties levied against LHH related to the 2019 patient sexual abuse scandal, and lawsuit settlements awarded to plaintiffs who sued LHH for that scandal. The $8 million is expected to climb rapidly over the next four months, because 1) The “Tommy Thompson et al.” class action lawsuit settlement is expected to add another $2 million, if not more, when the Health Commissions is expected to approve the settlement in the coming weeks, and 2) Three post-discharge wrongful death lawsuits following the July 2022 evictions of 57 LHH residents are expected to go to trial between November 2025 and January 2026, with settlements likely offered beforehand to spare the City from public scrutiny during jury trials.
 Importantly, that $8 million in costs will increase significantly when the four settlement amounts are released, and associated City Attorney time and expenses are made public from litigation cases. Unfortunately, the costs of City Attorney time and expenses fighting CMS ever since 2021 and LHH’s decertification in April 2022 may never become known because that didn’t involve actual litigation.
Importantly, that $8 million in costs will increase significantly when the four settlement amounts are released, and associated City Attorney time and expenses are made public from litigation cases. Unfortunately, the costs of City Attorney time and expenses fighting CMS ever since 2021 and LHH’s decertification in April 2022 may never become known because that didn’t involve actual litigation.
That’s because in response to a records request, the City Attorney asserted on August 8 that specific sections of California’s Government Code, Evidence Code, and Code of Civil Procedure, bars release of that data, saying:
“Please note that we have no disclosable responsive records. Our billing for advice matters [to individual City Departments] outside of litigation is exempt from disclosure under the attorney-client privilege and work product privilege.”
We’ll never know the total costs of City Attorney time spent on non-litigation matters between April 2022 — when LHH was decertified — and now trying to keep LHH from being closed down completely. Over the past three years, its probable the City Attorney’s time representing LHH outside of actual litigation and including trying to save LHH’s 120 beds has easily been several million dollars.
A third chart summarizes $8 million in salaries for five LHH and San Francisco Health Network employees who played leading roles in the LHH decertification effort, which has now led to the long-term loss of 120 beds at Laguna Honda. The chart includes the $20,000 monthly pension star-of-the-show Mivic Hirose now earns (totaling $524,706 since her retirement from City employment in June 2023).
Their five roles in this stage drama are described below.
Decertification Could Have Been Avoided
Troy Williams and Grant Colfax’s failed 2019 eight-page “LHH 60-Day Reform Plan” — including a two-page Appendix listing the CMS deficiencies cited in response to the patient sexual abuse scandal in 2019, which Appendix SFDPH deliberately “scrubbed” out of the six-page “Reform Plan” available to this day on SFDPH’s website in a gaslighting attempt to “disappear” that data — shows the anemic “reforms” LHH attempted in 2019. Those reforms were a complete failure, and led to LHH’s decertification three years later. Williams should have been let go, then and there.
 Had their reform plan worked, LHH might have course-corrected following the 2019 patient sexual abuse scandal, and LHH may never have become decertified and it could have been avoided completely.
Had their reform plan worked, LHH might have course-corrected following the 2019 patient sexual abuse scandal, and LHH may never have become decertified and it could have been avoided completely.
The principal players in this tragedy-of-errors included Mivic Hirose — who admitted to a California patient safety inspection team, in front of a San Francisco Deputy City Attorney, that under her watch as LHH’s CEO, she had failed to institute a “culture of safety” at LHH. Hirose had come to LHH after having reportedly begun her career at San Francisco General Hospital as an operating room surgical nurse.
Then there was Director of Public Health Grant Colfax, who had become Director in February 2019, just five months before the patient sexual abuse scandal erupted at LHH’s. Colfax’s career up to then had been as an HIV/AIDS policy wonk.
Third up, was Troy Williams, who began as a Licensed Psychiatric Technician at SFGH in April 1995, advanced to being a Staff Registered Nurse in Inpatient Psychiatry, then a Nurse Manager in Psychiatric Emergency Services, and eventually into being SFGH’s “Chief Quality Officer” in 2014 after working as a Director of Risk Management in SFGH’s Quality Management Department, a role that nurses often grow into to escape performing direct patient care with combative patients. Instead of being canned for the failed 2019 “60-Day Reform” plan for LHH, Williams is now the “Chief Nursing Officer” and “Chief Quality Officer” for all of SFDPH. Since he’s worked for SFDPH for now 30 years, hopefully he will retire soon. He should join the ranks as another nurse drawing a $20,000-plus monthly pension, like Hirose!
Baljeet Sangha began his career at San Francisco General Hospital as an intern in its materials management department, and climbed the ladder to being Chief Operating Officer for the San Francisco Health Network. Sangha had been befriended by Delvecchio Finley, who served at one point as LHH’s Chief Operating Officer but wasn’t widely regarded, instead widely ridiculed.
Despite both men never having had experience running skilled nursing facilities or expert knowledge of CMS’ nursing home regulations, Sangha and Williams were inexplicably appointed as “LHH Recertification Co-Incident Commanders” to help rectify the issues at LHH that led to its decertification by CMS. How do you rectify problems you have no experience with?
As it was, Williams’ 2019 “60-Day Reform Plan” had stated LHH would pursue accreditation from “The Joint Commission” (formerly known as “JCAHO”). Williams hadn’t understood in 2019 that JCAHO accredits hospitals, and that was inapplicable to LHH, a skilled nursing facility.
And finally, there was Roland Pickens, who was chief operating officer of San Francisco General Hospital in 2010, and moved into a cushy hospital administrative job with the San Francisco Health Network when it was created around 2014.
 None of these five key employees had any training in running a skilled nursing facility, and indeed in mid-2023, Pickens publicly admitted that even after he became acting CEO of Laguna Honda, SFDPH managers had continued to run LHH as if it were an acute-care hospital, not as a skilled nursing facility. Oops!
None of these five key employees had any training in running a skilled nursing facility, and indeed in mid-2023, Pickens publicly admitted that even after he became acting CEO of Laguna Honda, SFDPH managers had continued to run LHH as if it were an acute-care hospital, not as a skilled nursing facility. Oops!
The link above to the paltry six-page 2019 “Reform Plan” written largely by “quality expert” Troy Williams that Director Colfax had lent his name too, didn’t work as planned and LHH was decertified three years later. It took until four years later in 2023 when LHH — well into a year of decertification-related corrective actions — finally hired Sandra Simon, who held a Nursing Home Administrator license and knew what she was doing, as LHH’s CEO.
An AI analysis of Williams’ 2019 “60-Day Reform Plan” is scathing, reporting the plan was started in response to the 2019 patient sexual abuse scandal at LHH to address regulatory findings — skilled nursing facility findings Troy Williams had no experience with. The plan proposed reorganizing LHH’s Quality Management Department, which Williams purportedly had experience with. The AI overview generated by Google’s generative AI tool, “Gemini,” correctly reported:
“Public records and reports indicate the plan was largely considered a [complete] failure and didn’t prevent LHH’s eventual decertification by the Centers for Medicare and Medicaid Services (CMS) in 2022. Critics argue that LHH continued operating more like an acute-care hospital rather than [like] a skilled nursing facility, and that leadership failures contributed to the plan's ineffectiveness. These issues eventually led to significant costs to the city in fines, penalties, lawsuit settlements, and consultant expenses related to LHH's recertification efforts.”
 Apparently, Troy Williams had concluded in 2019 that LHH’s problems were mainly confined to its Quality Management Department. (Spoiler alert: They weren’t!)
Apparently, Troy Williams had concluded in 2019 that LHH’s problems were mainly confined to its Quality Management Department. (Spoiler alert: They weren’t!)
AI tools appear to be smart enough to realize this complete failure was the direct result of leadership failures. Those leadership failures include — but are not limited to — the five people named above, plus San Francisco’s Health Commission, in particular Commissioner Edward Chow, MD who is confused about whether LHH has 649 remaining beds, or just “500-plus.”
Hope for the Future?
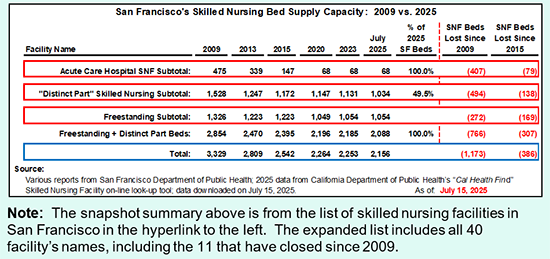
As another chart shows, San Francisco is down to having just 2,156 skilled nursing beds in-county, after losing 1,173 such beds since 2009 involving losing 386 such beds since 2015, including the new loss of 120 beds at Laguna Honda, that we couldn’t afford to lose. That exacerbates the number of San Franciscans “granny dumped” into out-of-county skilled nursing facilities across the past three to four years, which will be explored in an upcoming September Westside Observer article.
 But wait, there’s more. We haven’t heard a peep out of San Franciso’s Board of Supervisors, who have now high-tailed it out of town for their month-long August recess. They are complicit in this mess, too, because the Board of Supervisors have shamefully only held three hearings on the crisis at Laguna Honda since it was decertified in 2022, thanks in part to Supervisor Myrna Melgar’s failed “leadership” as District 7 Supervisor where LHH is located. She’s much more focused on getting Mercy Housing’s 110-unit senior housing project built on Laguna Honda’s campus, rather then protecting LHH’s 120 skilled nursing beds. The entire 11-member Board of Supervisors are completely missing in action about LHH!
But wait, there’s more. We haven’t heard a peep out of San Franciso’s Board of Supervisors, who have now high-tailed it out of town for their month-long August recess. They are complicit in this mess, too, because the Board of Supervisors have shamefully only held three hearings on the crisis at Laguna Honda since it was decertified in 2022, thanks in part to Supervisor Myrna Melgar’s failed “leadership” as District 7 Supervisor where LHH is located. She’s much more focused on getting Mercy Housing’s 110-unit senior housing project built on Laguna Honda’s campus, rather then protecting LHH’s 120 skilled nursing beds. The entire 11-member Board of Supervisors are completely missing in action about LHH!
The fewer steps Director Tsai, Mayor Lurie, and San Francisco’s City Attorney take to protect the supply of skilled nursing facility beds in San Francisco, the more responsibility they will bear for the loss of even more SNF beds in our City, along with the skyrocketing number of out-of-county discharges there will be for San Franciscans who need SNF level of care following hospitalization for acute care.
 LHH’s long decades of a culture of mismanagement now includes mismanagement in abandoning saving 120 of LHH’s beds. This can’t wait until a nebulous “at some future point” — assuming some change in the Federal government — or an even more nebulous “proactive efforts and alternative pathways.”
LHH’s long decades of a culture of mismanagement now includes mismanagement in abandoning saving 120 of LHH’s beds. This can’t wait until a nebulous “at some future point” — assuming some change in the Federal government — or an even more nebulous “proactive efforts and alternative pathways.”
Currently, there’s little hope LHH’s 120 beds will be saved anytime in the future, or that Director’s Tsai prayers for “alternative pathways” will come to fruition.
Two wrongs, obviously, don’t make anything right.
Growing old in San Francisco includes dying from side effects, that Barbara Ehrenreich’s book, “Natural Causes,” addressed.
Monette-Shaw is a columnist for San Francisco’s Westside Observer newspaper, and a member of the California First Amendment Coalition (FAC) and the ACLU. He operates stopLHHdownsize.com. Contact him at monette-shaw@westsideobserver.com.